There are many factors that influence the long-term retention of critically essential teeth. Certainly, endodontic procedures pose treatment considerations when performing restorative dentistry...
The Restoration of the Lost Papilla Special Guest Presentation by Dr. Jean Wu
The show begins with a short baseball rules analysis, as autumn is in the air and the World Series is fresh on our minds. This is then followed by our special guest, Dr. Jean Wu, a Newport Beach prosthodontist who gives a presentation on restoring the lost papilla. After, Ruddle and Lisette share insights in a post-presentation discussion. The episode ends with the exploration of another unsolved mystery…beyond the average endodontic conundrum! This time we are off to the Scottish Highlands, the home of the Loch Ness Monster.
Show Content & Timecodes
00:34 - INTRO: Baseball Rule Changes – Past & Proposed 11:54 - SEGMENT 1: Guest Presentation by Dr. Jean Wu 52:27 - SEGMENT 2: Post-Presentation Discussion 58:54 - CLOSE: Unsolved Mysteries – Loch Ness MonsterExtra content referenced within show:
- Special Guest: Dr. Jean C. Wu
- Sheets, Wu & Paquette practice website: www.sheetsandpaquette.com
- Newport Coast Oral Facial Institute: www.ncofi.org
- Academy of Microscope Enhanced Dentistry: www.microscopedentistry.com
- The Western Society of Periodontology: www.wsperio.org
- Ladia O, Ntovas P, Gogolas N, et al: Impact of Long Contact Areas for the Management of Varying Levels of Interdental Papilla Loss on the Perception of Smile Esthetics between Dentists and Laypersons in Asymmetric and Symmetric Situations, J Prosthodont 34:5, pp. 478-489, June 2025
- Tarnow DP, Magner AW, Fletcher P: The Effect of the Distance from the Contact Point to the Crest of Bone on the Presence or Absence of the Interproximal Dental Papilla, J Periodontol 63(12), pp. 995-6, 1992
- Nordland WP, Tarnow DP: A Classification System for Loss of Papillary Height, J Periodontol (10), pp. 1124-6, 1998
- Kataoka S, Nishimura Y, Sadan A: Nature’s Morphology – An Atlas of Tooth Shape and Form. Quintessence Pub. Co, 2002
- St. Adamnan’s Biography – The Life of Saint Columba, 7th Century
- “The Private Life of Sherlock Holmes” – Comedy/Thriller Movie, 1970
‘Ruddle Show’ episodes & podcasts referenced within this episode:
- Find referenced shows within the You May Like tab above
Downloadable PDFs & Related Materials
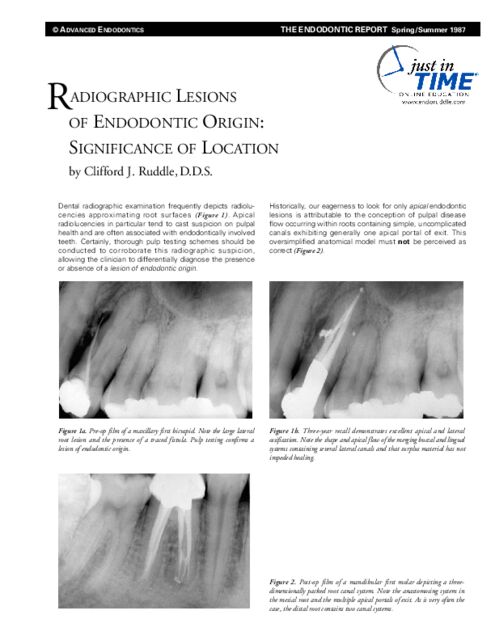
Dental radiographic examination frequently depicts radiolucencies approximating root surfaces. Apical radiolucencies in particular tend to cast suspicion on pulpal health and are often associated with endodontically involved teeth...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
OPENER
…They did not find a monster, but they did pick up on three sonar contacts that indicated quote “something big”…
INTRO: Baseball Rule Changes – Past & Proposed
Welcome to The Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How you doing today?
I’m doing pretty good, how about you?
Never better. And I want to welcome everybody to another show. We have some fun stuff, so get us started.
Okay. So when autumn comes around, a lot of us think of Halloween or back to school. But there’s also the fall classic, also known as the World Series. Our viewers probably know that we really love baseball, so we’re going to take a moment to talk about what’s happening. The playoffs are under way.
So in my household there’s been a lot of heated discussion, and actually sometimes just outright anger about how the home plate umpire is calling balls and strikes. The problem is that you see the strike zone box on the television and you see the pitches come in. But then you’ll notice if you watch a few pitches, the calls that the umpire is making don’t always match the visual evidence. So what the heck is going on here?
Well, being an old timer, I can tell you that baseball has had this dilemma as long as I’ve been watching baseball. The dilemma is every umpire has more or less their own strike zone. Forget the usual rules of what defines the strike, you know, the letters, the knees, the plate width; they have their own strike zone. Batters adjust to that nicely if, in fact, it’s consistent. So if the referee/umpire is consistent across nine innings, everybody’s happy. The problem is there’s a lot of inconsistency, even among the same umpires, changing zones.
So to address that, baseball for next year, 2026, is going to have a challenge system. It’ll be an automated one and you get two challenges per game. Apparently it’s the catcher, the pitcher and the batter, and those are the three that can, in fact, make the challenge. If you lose your challenge, you lose your challenge and you now have one left. If you win your challenge, you get to maintain your challenges.
I’m wondering if you can have more than one challenge at a single at bat. But that’s just something – I don’t know if you know the answer – but I was just wondering about that myself.
I don’t know.
Well that sounds like it actually would be a good system to implement. I kind of tend to want to just have a fully automated system, but I guess this sort of transitions to make everybody a little happier. And I guess actually this is what players and umpires voted for; this challenge system versus a fully automated system.
Yes. I think baseball purists probably don’t want any of this in there. But I think the younger kids coming up, and I mean like the last two or three decades, they probably would like that. When you see it in tennis and you see it in other sports, electronic line calling, you’re just going why can’t we have that kind of consistency at the plate?
Okay, well there’s also been some other recent rule changes that have taken effect in just the last few years that have really had a positive impact on the game. What are those?
Games dragged on too long. They were approaching three and a half hours easy, sometimes close to four. So they want to speed things up, make it more urgent and exciting, and not so much of a yawner. So they got a pitch clock. There’s a pitch clock for the pitcher, and then there’s also a number of seconds given to the batter. So it keeps things moving.
They made the bases bigger. They used to be 15 inches on a square, now they’re 18. So as you pointed out to me, if you move one base out three inches and we move this one back three inches, we’ve closed the distance from first to second as an example six inches. And a lot of calls, as you know, are boom-boom, and that can make a difference in steals. So that was good.
Shifts that our players used to – if there’s a pole hitter up, and maybe you don’t know what that means overseas or somewhere, or even in the United States; probably a lot of people don’t even know what that means. But if you’re a guy that likes to rip the ball down the lines, whether you’re a lefty or a righty, sometimes teams defensively would shift their whole infield over, like say between second and third if it’s a lefty at the plate. And they might even have one of those four people playing in the outfield, like a shallow right field. And that got to be kind of boring and over stacked, so now they want two players on each side of second base and on the dirt. So that probably averages it out better. You could argue why can’t the damn batter learn to punch the ball down the open infield, but that’s another whole day.
And then finally pitchers. There’s a lot of changing pitchers, and that drags out with advertisements and stuff; the new guy comes in and has to warm up, gets so many throws. So now if you bring in a pitcher you have to either finish the inning or face a minimum of three batters.
Okay, well those sound good. I watch a lot of baseball, and as I’m sitting there watching, sometimes some change in rule suggestions pop into my head. So I thought maybe, just maybe the Commissioner of baseball is watching The Ruddle Show right now, and this is kind of my chance to put out my suggestions. So do you mind if I do that?
Go right ahead, I’m dying to get – I mean change is inevitable, right? So what have you got?
Okay, let’s go to the side set and we can look at those.
Okay. Now that we’re over by a baseball diamond; it’s time to play ball.
Okay, so the first suggestion I have is called “double or nothing.” And maybe you can help me draw it out for the visual part.
So say you’re a base runner on third and you’re running in to home plate. You can either choose to run straight through and get one run, like normal. Or you can choose to try for two. And you would round home plate and head back to first, assuming first base is open.
Then if you got out though at any time when you’re running the bases for the second time, you would get zero. And if you got out, or if the inning ended before you made your second time around, you would also get zero.
So the idea is that if it’s late in the game and you’re behind, then maybe you have the opportunity to try to get two runs instead of just one. Or if you have zero outs and you want stay a base runner, then you can try for two. So that’s my first suggestion.
Well I’ll just add one thing. Everybody that plays baseball, and it’s played internationally, so if the runner comes down the bag and makes any turn whatsoever, any commitment, they’re a live batter. So if this guy that she’s proposing is on third, or could even be on second trying to come in; if they go through the plate and go towards the dugout, they got a run. But if they turn, just like if they turn to the left, they’re a live runner; and any throw from the infield, shortstop anywhere, can gun them down at first base.
Right. So this might require a little bit of change in the field design to allow for a rounding.
You might have to mow the lawn back, get a little dirt here. Because just like you make arcs going around these bases to make it the most efficient trip possible, you couldn’t just come down here at full speed and make a 90. So yeah, I like your idea.
I think it would make the game exciting. Because whenever you get someone on base and you have a baserunner, it’s exciting.
Well we’ve had some close World Series games, so probably that could have made a difference.
Yeah. My second suggestion is called, I call it the “double play carry-over.” So say you’re on defense, maybe it’s the top of the third, and you already have two outs. And then you get a double play. Well the third out would happen; that would end that inning, or end that half of the inning. And then the next time you started on defense, the top of the fourth, you would already start with one out. So it would carry over.
I see.
So there’s that. And then the last one that I -
Well I wanted to comment on that; that’s pretty good. So in other words, you’re saying this extra out that you could get. I just want to say there can be more than one runner. In this idea, all the runners have to be part of the signaling and coaching and base path running because they don’t want to get thrown out, they’re all live.
Yes. And also a lot of times you just do the easy throws to first, to get the easy out.
To force the out.
Yeah, to get the easy out because that will end the inning. But it makes it kind of exciting if they’re trying for a double play and maybe they make an error because double plays are a little more risky. So then that would just encourage excitement in the game.
The only thing that threw me a little bit about your idea was you said when there was two out and they go for a double play. That would be the new rule right there, because when there’s two outs, you just shovel the ball to second or third, wherever there’s a force, and take the easy out and you’re out of the inning.
Right. But you would just carry over - if you got a triple play, it would carry two runs over.
Oh, I like that.
Or two outs.
A new kind of baseball.
All right. And then the last one I call the “hit by pitch ladder.” So this doesn’t matter. It’s like say a pitcher hits the batter. Well we all know the batter takes first base. Well say it happens again. Even if it’s a different pitcher but it’s the same team that’s hitting a different batter, then that next – the second hit by pitch would take the batter all the way to second, and moving runners along too.
Yup. Two times you get to go to second. You get hit one time you get first; twice, second. Three pitches you said – we’re over here – three times.
And so here you have -
Well what about the fourth?
Okay, so here you have a situation. If the bases are loaded and your team has already been hit by the pitch three times in the game -
Oh gosh!
Then a fourth one, it’s possible to get a hit by pitch grand slam.
Three runner.
A hit by pitch grand slam is a possibility. Those are my suggestions.
I don’t know. Maybe you could write in and let us know if there’s anything we missed, or if you have other self-evident rule changes that could prosper.
So what did you think?
Well I’m going to have to think about a couple of those. Because one thing that your rules are; they’re logical, but it implies that a lot of the people on base have to know what’s going on.
Yeah. I mean there’s already a lot of people that don’t understand all the intricacies of baseball, so maybe it would just overcomplicate things. I don’t know. I think it might make it more exciting.
You know, my daughter Eva was just talking with her boyfriend the other day about baseball. And he said oh, baseball is really boring. And Eva said well it’s not in my house actually. It gets quite emotional, there’s a lot of ups and down. Yeah, I love baseball, and I know you do too.
Well yeah. But I guess I’d say in closing that baseball, which has been played since the 1800s; if they can implement changes, maybe in endodontics we could implement changes too. Beyond the technology. Like maybe we could actually train up a little bit and we could be more effective and have more fun.
Okay, well we have a great show today. We have a guest speaker, so let’s get to that.
SEGMENT 1: Guest Presentation by Dr. Jean Wu
Okay, today we have a guest presentation which you will see momentarily. It is by Dr. Jean Wu, who is a prosthodontist in Newport Beach. She is a partner in the Sheets, Paquette and Wu Dental Practice, which is known for providing the finest dentistry in a very caring and professional environment. Dr. Wu is very passionate about her work, and her journey has emphasized helping the less fortunate and those in need.
So the title of the presentation that we’re going to see today is called The Restoration of the Lost Papilla Using Collaborative Efforts. But before we watch it, maybe we do the usual. You tell us how you know Dr. Wu and how it came about that we have the opportunity to show this presentation today.
Thanks. You kind of set me up. Since I have been friends with Cherilyn Sheets for several decades, and you mentioned that Wu, Sheets and Paquette are in the same building. I used to go down there quite a bit to the – it’s called the Newport Coast Oral Facial Institute, and I used to go down there quite a bit and just hang out. A lot of our InnerView meetings and that technology were down there with the engineers. And so I was in and around, but just saw her from a distance and there was no formal hugs or anything like that.
And then we both co-presented, I believe, in 2023; yup, 2023. It doesn’t matter really, but recently, 2022. And it was the Pacific – it was AMED; it’s the Academy of Microscope Enhanced Dentistry, and the Western Society of Periodontics. So there was a joint meeting between those two groups and we were both presenters. And at that time we did speak more, got to know her a little bit better.
And then finally she got asked to be the president of the Pacific Coast Society of Prosthodontics, and she asked me to be one of the keynote speakers. So we talked quite a bit about what she wanted me to do and I got to meet her and we talked, and out of that came a relationship. And of course I was very fascinated by her journey. I was fascinated by Josette Camilleri; her journey was quite remarkable I thought. And this one was a journey that started in Taiwan, then it went down to Melbourne, Australia, off to Pittsburgh, Pennsylvania, and finally the West Coast.
So yeah, she’s quite a traveling lady.
Okay, so great. Well my introduction of Dr. Wu is going to be brief because she gives an excellent first-hand account of her own professional journey at the beginning of the presentation.
Yes she does.
I just want to add though that she is a past president of the Australian Prosthodontics Society, the Pacific Coast Society for Prosthodontics, and also the Academy of Microscope Enhanced Dentistry, which you mentioned.
I had a hard time with that didn’t I?
She is a distinguished international lecturer and clinical instructor, she has published several scientific papers and collaborated on chapters in textbooks about implants and materials. And I’m still only saying a little bit; you should check out her complete bio in our show notes if you want to know more.
So needless to say, we are very honored to have the opportunity to show this presentation today, so let’s watch it.
[Wu Presentation Begins]
Hello everyone. So nice to be here to join you for The Ruddle Show. Such an honor to be asked by Dr. Cliff Ruddle to present to your esteemed group. I hope you’ll find my presentation interesting. Let me tell you a little bit about my background.
I grew up in Melbourne, Australia; I continued to receive my dental education at the University of Melbourne, Australia. After one year in a general practice residency in a major medical center, I then went on to doing prosthodontics at the University of Melbourne, Australia. And during that time I felt that I could help the more needy, such as children with cranial/facial deformities and trauma patients, patients with cancer and other debilitating diseases that resulted in a defect in the oral cavity.
So I wanted to know how to make obturators. I wanted to know how to reconstruct face defects. I also wanted to work with children and see where I could help as a prosthodontist to reconstruct cleft lip and palate patients, ectodermal dysplasia, hemifacial microsomia, children who’ve had other oral cancers resulting in oral defects, because I knew that without us, patients with these defects could not speak, could not drink, could not eat. Newborn babies could not feed.
And so we were taught how to take impressions in babies who were just a few hours old, and we could make a very simple base plate to allow them to create some negative pressure to suckle and feed. I found that most rewarding, and that took me to the University of Pittsburgh where I did a maxillofacial residency. And during that year I saw trauma patients, motor vehicle accidents, gunshot wounds, and other pretty debilitating traumatic incidents which result in areas of their oral/facial structures being damaged. I also was honored to be part of the Regional Center For Cleft Lip and Palate at the University of Pittsburgh, and there I was able to help treat many cranial/facial deformities. I was also able to be part of the tumor team and was able to participate in reconstruction of patients with various oral cancers.
So that led me to the United States. I met my husband at the University of Pittsburgh, and then I joined the faculty at the University of Tennessee in the fixed and removable restorative department. During that time I was also able to obtain my international DDS degree, and then able to get my California license, and then joined the office of Cherilyn Sheets and Jacinthe Paquette in 2002. There I have practiced in private practice, as well as taught in the Newport Coast Oral Facial Institute. At this non-profit center we teach dentists how to use the clinical microscope, treatment planning, tooth preparation, and we also have visiting alumni such as Peter Nordland teaching periodontal surgery, endodontists like Dr. Ruddle. And it really is an ability for us to share our knowledge using the clinical microscope in various areas, various specialties.
So with that, I would like to share my presentation and I hope you enjoy it.
So today I’d like to share with you a presentation focused on how to restore the missing papilla. So the missing papilla can create esthetic concerns as well as functional compromises for the patient. So today the topic of my restoration is how do we collaborate and restore the lost papilla? We can use a combination of surgical, orthodontic, direct and indirect methods. This was presented recently at the Western Society of Periodontology and the Academy of Microscope Enhanced Dentistry on September 13th in California.
I have no disclosures and no affiliations that affect the objectiveness of my presentation today.
So why is the missing papilla important to us, the clinician, and patients? Most patients will present complaining of the black triangle. Clearly the esthetics of a missing papilla is a compromise during social function and appearance. In this case you can clearly see the dark, black triangles where there was missing interdental gingiva.
We can also appreciate the compromise in phonetics and speech, where there is air escape and also sometimes saliva escape. So it makes it difficult for patients to talk sometimes when there is missing gingival papilla.
Plaque control can also be difficult, as there is a larger embrasure form for patients to maintain and clean and remove the plaque. And oftentimes staining is also more prevalent. Food impaction in these triangles is also a concern for some patients, but clearly most patients are most concerned with the appearance of these dark spaces and embrasures.
In a recent article in the Journal of Prosthodontics, in June of 2025, there was a study surveying how the loss of the papilla and altering the coronal contact point and crown contour would affect the perception of the smile and esthetics, between professionals (dentists), and also lay persons, when the missing papilla was on one side and it was asymmetric, and also when the missing papilla was on both sides. So if only one central incisor was altered to close the papilla, it was perceived as more unattractive, more unesthetic than if both the centrals were restored. And so oftentimes that would be ideal for patients to have both centrals modified to enclose or close the triangle or restore the missing papilla. In addition, if there were increasing, long contact areas, that was perceived as less attractive than if it was only slightly modified to close the missing papilla space. So the greater the defect, the more unattractive or more esthetic compromise was perceived by both lay persons as well as dentists.
So what factors can affect or cause a missing papilla? Clearly periodontal disease affecting the osseous structure or osseous crest height will result in a missing soft tissue embrasure missing papilla. In this pivotal, landmark article in 1992, Dennis Tarnow and others studied the distance between the contact point and the osseous crest. The further away the contact was from the osseous crest, a critical 5mm distance, the greater the likelihood that the papilla would be missing. Therefore, if the contact point was less than 5mm away from the osseous crest, there was more likely to be papilla fill than if the contact point was greater than 5mm away from the osseous crest. Therefore, if we were to modify the location of the contact point, such as modifying the crown contour and creating a longer contact point, then we could be more effective in closing that defect or camouflaging the area of the missing papilla.
The tissue biotype would also affect and result in greater papilla loss. Thin biotype, low osseous crest, will result in a larger embrasure defect and create a greater missing papilla; as opposed to a thicker biotype with a high osseous crest. In this situation, the patient had tapered clinical crowns, as opposed to square, more rectangular crowns, causing a larger black triangle or more defect with her missing gingival tissues.
Peter Nordland and Dennis Tarnow in 1998 also had a classification system that they documented in the Journal of Periodontology. They classified the Class 1 papilla defect as that where the papilla tip was coronal to the interproximal CEJ. A greater defect such as the Class 2 papilla defect was when the tip of the papilla was apical to the interproximal cementoenamel junction. The largest, most severe defect, classified as Class 3, was when the tip of the papilla was apical to the facial CEJ, and that was the most severe classification category. And this would be an easy way for us to communicate with our colleagues when we’re describing the defect caused by a missing papilla.
What are some of the factors that affect or cause a missing papilla or soft tissue defect? Parafunctional habits often can cause recession, bone loss, and result in the missing embrasure form or soft tissue fill. Occlusal discrepancies such as non-working or balance interferences could also result in hard tissue loss, bone loss, and also soft tissue or gingival tissue recession. Clearly, periodontal disease can result in damaging the hard and soft tissues and cause recession and a resulting missing papilla.
In this case that I will describe to you, the systemic health of the patient was also compromised by a pre-diabetic, Type II diabetic condition, where she was recently diagnosed with a metabolic defect that resulted in her soft tissue and inflammation levels and increasing recession and tissue loss. These patients need to be clearly treated so that we can stabilize the Type II diabetes, and also put her on a strict regimen where there was plaque control, deep cleaning if it was necessary. In this case she didn’t have any deep pockets; it was more supragingival plaque and staining and calculus that needed to be managed, and we need to keep these patients on a very close recall so that we can treat their diseases as they reoccur.
So what treatment modalities do we have to restore the missing papilla? The ideal treatment would be surgery if we can restore the soft tissue defect with the patient’s autogenous gingival tissues, such as from the palate, and connective tissue grafting. If surgical measures were unsuccessful or not possible, we could use orthodontic measures to close these embrasure areas, modify the coronal contours, so that we can bring the roots closer together. That would be another natural way that we can close the embrasure area where the missing papilla is requiring attention.
The third option would be to use a restorative or direct composite restorations to close the black triangle. Systems such as the Bioclear System where the matrices are ideally contoured and not flat, would be an ideal way to use direct composite material to close these black triangles. It would not require any removal of tooth structure, and can be very effective. Perhaps there will be a presentation in the near future from David Clark, the inventor of the Bioclear Matrix System.
Today I will be presenting indirect restorative techniques, such as using porcelain restorations, porcelain veneers, porcelain crowns, to close the black triangle or restore the missing papilla. This patient presented complaining of embrasure form where she was missing the papilla, creating base dot triangles. She has some minor Class 1 malocclusion where she had some mandibular crowding. She requested not only the black triangles to be closed, but to modify the shade of #7, which was a non-vital endodontically treated tooth, as well as a non-vital #8 which looked slightly darker than #9, which was also endodontically treated. She also had some discrepancies with the gingival levels of tooth #8 compared to 9, and there was some minor gingival sculpting that was performed after orthodontic treatment. And then finally, porcelain veneers to address the shade discrepancies as well as close the black triangles.
So orthodontic treatment was completed. The goals of the orthodontic treatment were to establish a mutually protected occlusal scheme, remove the balance interferences and non-working contacts, and idealize a restorative space so we could accomplish the widening of #7 and #10 as the patient desired a balance between the width of the laterals and the width of the central incisors.
So this is how the patient presented post-orthodontic treatment. You can see that the gingival crest was also idealized so the level between 8 and 9 was more even, and she was ready for her indirect restorative planning. You can see in this picture, her right lateral exclusive movement showing canine guidance between #6 and #27, elimination of balancing interferences where she had some non-working contacts on the contralateral side. We also established anterior guidance to disclude using the incisors so that the posterior teeth were not overloaded, and we also increased the width, or the restorative space, to allow us to increase the width for #7 and #10.
You can see in this short video the example of a veneer preparation on another patient, where this patient requested idealizing the length of the lateral incisors post-orthodontic treatment, as he felt that #7 and #10 were diminutive and undersized. This is just giving an example of giving a veneer preparation where we do reduction guide initially; using the reduction burs to create an ideal .8mm or 1mm space for the porcelain veneers. And this also shows a double view of retraction cord to move the soft tissue away from the margin preparation, to allow us to create a little deeper, interproximal finishing location of the margin. This allows the ceramist or the technician to create a more idealized emergent profile on the mesial and distal, to optimize the closure of the embrasure form.
Also, this shows the provisional restoration in place and the location of the emergent profile interproximal to close the area where there was a small missing papilla, which bothered the patient. And hiding the finish line to the lingual aspect so that we don’t have any discoloration and staining at the veneer margin. So it requires a preparation that goes to the lingual and involves the interproximal contact area.
So this picture from the Atlas of Tooth Shape and Form published in 2002 is just to illustrate the importance of the proximal transitional contour. It’s not flat. It’s curved so that we have a more natural crown contour. And it also allows us to create a mesial or distal marginal ridge so that the tooth doesn’t look too wide in the interproximal area where we’re trying to close the interproximal contact. By moving this marginal ridge, we can create shadows and light reflection so that the tooth is not perceived as too wide. So by moving the marginal ridge towards the center or the line angles, the tooth will look more narrow. If we move these line angles more to the mesial or distal, towards the interproximal contact, then the tooth will be perceived as more wide.
In the crosshatch area in this diagram, if the technician can shade the veneer or shade the crown to be a little darker, it will give you the illusion of depth so that the restoration is not too unnatural or too over contoured. And the tooth can still look natural as the shading in the mesial and distal area will allow the tooth or the restoration to look too over contoured, which is required to close the missing papilla, embrasure, or close the black triangle.
You can see in this case, the preparation design had to go to the lingual; the contact area had to be involved as you want to hide the finish line of the veneer on the lingual. You can also appreciate that the mesial and distal marginal preparation had to be a little deeper to allow the ceramist to create an ideal emergence profile so that you didn’t have an overhung appearance or a half pontic appearance, that we could create the emergence in a smooth manner to close that embrasure area. So the tooth would still look natural and not bulky at the CEJ or the area where the missing papilla was involved.
So in this occlusal view you can appreciate that in the pre-operative photo on the left compared to the post-operative view, you can appreciate the finish line of the veneer is more to the lingual. It’s a little bit deeper to create a more smooth transition that will minimize plaque accumulation and stain accumulation and food impaction. So these special details are what we need to include when we create veneers for closure of the missing papilla.
That is a little bit different from our conventional veneer preparation where we may not go quite as deep or as far to the lingual aspect, unless you are creating a color change. Therefore you’d want to create the finish line to the lingual so that you don’t show the dark, original preparation color.
In this case, a small porcelain veneer piece, or a partial porcelain veneer, was utilized to change the mesial incisal embrasure form to close the incisal embrasure. The patient felt the canine was too pointy. She also felt that the negative space between #6 and 7 was too wide in the incisal aspect. So this a partially seated porcelain partial veneer that could be utilized to change the shape of the canine without reducing it for a conventional veneer.
You can see in this view of the completed case in 2010 showing #6 had a partial porcelain veneer or porcelain mesial piece, #7 was a soft plastic porcelain veneer. Similarly #8, 9 and 10 were also soft plastic porcelain veneers to close the embrasure, missing papilla and large embrasures, as well as idealize the color match between 7 and 8 with the left #9 and 10. You will also note that #11 had a partial porcelain veneer to close the wide incisal embrasure, but not close it too much so that it looks unnatural.
In this follow-up photo from 2013, three years later, you can see that the soft tissue has matured. Sometimes that can take up to a year for the soft tissue to heal and fill in the embrasure areas between your porcelain veneers. It will just look better as long as the patient has meticulous plaque control and has strict hygiene recall. So her pre-diabetic state was also stabilized and her health had improved.
So you can appreciate three years later the optimal soft tissue health, as well as the esthetic appearance of the finished restoration.
So once again I wanted to highlight in 2010 after the veneers were immediately delivered, there was still some flat papilla interproximal contours; the soft tissue had not filled in around the new restoration. That takes time, and it could take many months and up to a year for that to be accomplished. And so in this follow-up anterior view, you can see how well the soft tissue had filled in and how it looked even more natural around the soft plastic porcelain veneers and the partial porcelain pieces on the canines.
This porcelain case was completed by Hiroki Goto, a master dental ceramist, in 2010 and follow-up in 2013. This other anterior view showing the lower incisors that had not been restored and were to be restored at a future date. You can see how the soft tissue was not ideal in 2010, but in 2013 had filled in and was improved. And you can note also in the lower arch, with meticulous oral hygiene and maintenance, the soft tissue around the lower incisors had also slightly improved.
Now in 2016 you can see the soft tissue fill in the maxillary incisors was still present, was perhaps a little less ideally filled than in 2013. Mandibular incisors were still stable. And in 2018 she had a little soft tissue remodeling and little less interproximal fill, but still acceptable to the patient and still improved from her original presenting condition in 2010.
But in 2025 there was a slight lapse in her periodontal maintenance. You could blame it on Covid that she was unable to attend the office and so there was an increased time between recall. Her hygiene was also slightly less desirable and less ideal, as you can see by the staining on the canine porcelain pieces. And so this highlights the importance of regular periodontal maintenance, stable medical condition of the patient. In this situation her pre-diabetic state had progressed. And so all those factors will affect the rate of gingival recession, gingival health, as well as the long-term stability of the patient.
This was how she presented in 2010 after the delivery of the restoration. And so clearly we need to go back and discuss how we can reestablish her to this level of esthetic presentation, as she is now not happy with the return of the interproximal embrasures that need to be addressed.
In this second case I wanted to share with you a slightly different presentation of the missing papilla in situations where the teeth are undersized. You can see in this example, in the pre-operative state, the maxillary incisors, and also you’ll see in a following view, the mandibular incisors were slightly undersized for the arch form. So the patient did not like the diastemas present and requested closure of the diastemas to improve the uniformity of her smile and remove the negative space created by the diastemas.
So you can see in this view the patient’s regular smile presentation. She had large diastemas, small maxillary incisors that bothered the patient, but the color of her teeth was not something that she wanted changed. She wanted the incisor translucency maintained. All she requested was larger teeth, to still look natural but to close the diastemas.
You can also appreciate the mandibular incisors were also slightly undersized, creating mandibular diastemas presenting between 23,24,25,26. Because of the difficulty of preparing lower incisors for indirect porcelain veneers, we elected to do direct composite restoration of the mandibular diastemas, but utilized porcelain veneers to restore the maxillary diastemas. In a lateral view, right lateral view of the preoperative condition, you can also see that there was some delayed passive eruption. She did decline crown lengthening, did not want any gingival surgery that would have idealized the smile and the lesser display of soft tissue, but she really only requested diastema closure and maintaining the shade or color, as well as the translucency on the incisal edges and the opalescence that was present in her natural tooth enamel.
In this close-up view, you can see how wide the diastemas were and how that created a very irregular, not harmonious appearance to her smile, which she found displeasing. And the incisal embrasure form was also lacking in uniformity, which is more desirable for patients as that creates the illusion of the teeth being more even.
You can see in this view of the conservative tooth preparation, we prepared the six maxillary incisors and canines for veneers. The closure of diastemas in the incisal embrasures required the finish line to once again be placed lingually, and once again to also be slightly subgingival to allow that ideal emergence profile of the final porcelain veneers.
This is a view with the matrices from the four diagnostic wax-up. To highlight, during the tooth preparation you can take an impression model, and within 10 minutes you can check your preparation, either with the in depth created on the full contour diagnostic wax-up. You could do a clear suck down material such as an Essex or a Viperline-like, clear matrices of the full contour wax-up, to show that you have an even reduction of the maxillary incisors. In this situation, the second plane was slightly under-reduced, as you can see by the red lines, and that required a little second plane bevel to allow the technician to have a more uniform thickness of the soft plastic porcelain.
With the gauge that you can see on the lower right corner of your screen, you can see that the porcelain veneers were .8 of a millimeter. So less than a millimeter in thickness as we did not require too much tooth preparation; mainly removal of interproximal undercuts and facial consistent reduction so that the thing, soft plastic veneers could be uniform in width or in thickness.
In this view you can see that the porcelain veneers created the incisal opalescence and translucency that the patient desired, but also followed the full contour wax-up matrices, as you can see in the purple. And this confirmed that we would follow the guidelines established before preparation so that we could allow the technician to build a uniform thickness in the soft plastic porcelain that would be more consistent in strength once it was laminated onto the enamel.
In this anterior occlusal view, you can see the margin location was more lingual in order to allow us to close the embrasures where the missing papilla or diastemas were to be closed, as well as a slightly deeper interproximal finish line to allow us to create that ideal crown contour or veneer contour. So you can see in this occlusal view how uniform the emergence profile was.
This view shows the porcelain characteristics of the opalescence in the incisal translucency. Once again, very beautifully created by our master dental technician, Mr. Hiroki Goto.
This is on the cast, the six maxillary veneers, and in this view you can see the lateral contours. Closure of the diastemas, idealizing the crown or tooth contours, but also closing the incisal embrasures so that we had a more harmonious, esthetically pleasing appearance to the maxillary tooth alignment.
You can see once the veneers were delivered, further soft tissue had to heal post cementation, but she once again did not feel concerned about the excessive gingival display and declined the periodontal surgery. But it’s still a very pleasing, uniform result, artistically created by Mr. Hiroki Goto.
You can see in this view, the mandibular incisors were addressed with direct composite restorations to close the diastemas, but the maxillary six incisors was created with soft plastic porcelain, once again so that we could create a more natural tooth forum that would not stain, she would not require as much maintenance of the porcelain veneers as she would require with the mandibular four incisors, which will need to be polished, may need to be resurfaced due to abrasion and wear. But it is definitely more conservative for direct restorations of smaller, undersized teeth that don’t require a millimeter or a .8 millimeter of tooth reduction.
She was very pleased with the result. It is exactly how she had desired to create a natural smile without the negative space of the embrasures of the diastemas, and close the contact areas and not have any dark spaces.
The third case I would like to share with you is a traumatic case where the patient had sustained an avulsion of tooth #7 and 8 over 25 years ago, and had dealt with endodontic procedures that were repeatedly required due to infection, and now she was undergoing resorption of tooth #6, #7 and #8. So in this case her extractions were staged and she would have a final restoration that was an implant supported bridge with an implant in site #6 and an implant in site #8, with a pontic in #7. But the stages were required so that we could manage the hard and soft tissue, manage the architecture and address the missing papilla, and create a more natural appearance.
So the implants were staged where #6 implant was placed first and #7 and 8 were utilized to support the provisional bridge. And then #8 was utilized; #8 was extracted once #6 was ready for provisional loading and 7 was still maintained. And then finally #7 was extracted when #8 implant was ready for provisional loading.
You can see the osseous defect created still after the staged extractions, where the crestal bone between the three extracted teeth was lost. And so in this situation, just utilizing tooth colored porcelain was not enough to restore the osseous defect. We would require some pink porcelain. You would appreciate how difficult Mr. Goto’s job was to match the contralateral enamel characteristics, which the patient really appreciated and wanted to maintain. So this is probably a very exciting day for the ceramists to express their artistic talent in trying to match what nature had created so beautifully.
You can see in the final restorative result, instead of just using tooth colored porcelain, pink porcelain was required to restore the missing hard and soft tissue, to allow Mr. Goto to create more ideal coronal contours to match the left natural teeth that were not compromised. And you can see the beautiful characteristics of the enamel that was recreated; a most challenging case because of the characteristics of her natural tooth color, but also challenging because of the osseous defect created from the surgery necessitated by the severe root resorption disease.
So the beauty of natural tooth color artistically created by Mr. Goto, recreated by Mr. Goto in this final result. And the patient was most pleased with the final appearance.
So I hope you’ve appreciated how indirect porcelain restorations can assist patients to close missing papilla embrasure forms, and create an esthetic result that is more pleasing and more uniform, and would also allow the patient to speak and eat more comfortably without these open embrasures collecting food debris, collecting stain, and also allowing air escape during function.
It was such a pleasure to be with you to discuss the restorative options to correct the missing papilla. So I hope you found it interesting, and please reach out to me if you have any questions. I look forward to seeing you again. Thank you.
SEGMENT 2: Post-Presentation Discussion
Okay, so I thought that was an excellent presentation; very clear and organized, and I personally learned a lot. I thought it was very thought provoking in a kind of philosophical way, the way she talked about esthetics in terms of both form and function. She talked about what is pleasing to the eye in terms of proportion, symmetry, contouring the shading, but then also a lot about functionality.
So I just thought that was very kind of philosophical. I was actually thinking a lot about where we talked on the podcast about those implant centers that do implants in one day. Versus all the thinking that went into what she’s doing. So there was quite a contrast there.
Oh yeah.
What did you think of the presentation?
Well if we’re talking about papillas and esthetics, I thought she nailed it really big time. And specifically how she managed – with prosthodontics she managed diminished or absent papillas alone; no surgery. Because in Santa Barbara we used to see people growing papillas, this was Dennis Shanelec. And Dennis Shanelec used to give classes on how to do grafts and slide pedicles and stuff. But this was great because through shape of the tooth in the end game, and with the size and the contours, the shading can be done. And if you put gentle pressure on a papilla, gentle pressure, you can actually have papillas grow.
So here’s the dimensions I learned from here. From the contact point between teeth to the crest of bone should be 5mm or less, and you can have a chance for papillas to merge into that space. If you’re greater than 5mm, you’re not going to do it with esthetic dentistry alone.
So that was interesting to note, and then of course you can’t just do all this dentistry as a stand-alone, one-man band; it takes a group, it takes a team. And she has – well it’s nice to have a certified dental lab technician, but even better would be a master dental technician. So she has a master, an MDT, master dental technician. His name is Hiroki Goto, and he is onsite, in the office, and he comes out with her while she’s working and preparing teeth. And they even talk about oh, reduce a little bit more over here because I can add more porcelain, and he uses incredible materials. He knows a lot about being artistic and he knows a lot about materials.
Exactly. She was referring to him sometimes as the master technician, and then other times she talked about him as a ceramist. So it kind of had a little bit of an artistic feel to it too.
I think that she really views her work as having both a technical aspect and an artistic aspect. And I think you kind of relate to that as well.
Well I do. You know, when we do beautiful endodontics, right? Schilder called it “the look” and the look meant that there were canals that were shape; they flowed and graced within the roots that them. There was a dimensionaless prep, but it was an appropriate prep. So the esthetic dentistry down below the bone, in the endodontic world we care a lot about that. And of course our work helps support their work, and if their work fails because our root canals fail then it’s all lost.
So yeah, I really related to the art, the science. I might be jumping ahead, but all this stuff they have, the MDT, they have the materials, they have the zirconia, they have the lithium type stuff and PFM type stuff. All that is over my head because the materials and the scientific endeavors have really massively forged forward.
But we have CBCT, we have microscopes, we have XNAV, we have different things that help guide our work below the bone.
How about what Hiroki Goto did with the pink porcelain to cover the osseous defect? That was pretty interesting.
As you all saw, there was the lady with the osseous defect; it was quite significant. And she had a high smile line, so when the lip came up you could see this. This was not going to be done with esthetic dentistry.
So what he did is he put a flange, a gingival, lining mucosa type polymer flange – porcelain flange I guess it really was. So when she smiles, it looked really quite normal. That was amazing.
Okay. I was pretty struck by that one case she showed, I guess it was the first case report, where the woman had a really good result from 2010 to 2018. And then everything by 2025 had drastically worsened, the perio, the staining. So that was a little disturbing that it got so bad.
You know I think we might look back and just be brutally honest. I mean when Covid hit in 2020, everybody stayed home, right? That was international. And so a lot of people changed their eating habits, their dietary habits. In other words not only eating habits, but what you eat. And then of course they blew off dental appointments, medical stopped. And so insulin can get out of control.
Right. I think she was pre-diabetic.
Yeah. So I think it was a matter of ceasing what she had faithfully been doing, and she got into a completely different routine and there was quite a relapse.
Yeah, I understand the importance of hygiene and regular appointments; that’s always been really obvious to me. And I also knew on an intellectual level that systemic disease affects your teeth. I just hadn’t really seen the visual evidence of it yet, so it was a little surprising to me. Any final comments?
Yeah. So Jean Wu does masterful dentistry, right? And I think many patients would say, if you asked them they would say; befores and afters, they’d say it was a miracle. But Jean Wu, you do ordinary miracles every day.
Right. Thank you again for that great presentation.
CLOSE: Unsolved Mysteries – Loch Ness Monster
Okay, so we thought it would be a good idea to close our show today with another installment of our Unsolved Mysteries. Previously we have talked about the infamous Alcatraz Prison escape, we’ve talked about what happened to Amelia Earhart, and then we’ve also talked about how and why Stonehenge was built.
Today we are taking this segment to the Scottish Highlands, to a long, thin lake called Loch Ness. So the legend is that a monster lives there, the Loch Ness Monster. So maybe you give a little background.
Well I’ve never been there and I’ve never seen it, so I can only tell you what we can all read or Google. But it’s long and narrow, about 23 miles. It’s amazingly deep, it’s about 800 vertical feet deep all along this channel. And so that’s kind of the setting.
I noticed that the monster stuff has been talked about forever, in my mind. And I guess in 565 A.D. there was an initial sighting, and then there was a follow-up biography that was written in the 17th what?
7th century.
7th century; geez, it was a long time ago – 7th century. And that was about the missionary the monk, St. Columba. And St. Columba was an Irish guy in Scotland, apparently checking out this lake, and he first saw something and reported in this book.
Then you have to go many, many – well hundreds of years, and you come up to the 30s, 1930s, and again, there’s more reports of it. And it’s interesting that this person that first saw it in the 30s said it was huge, it was black, it was big, and there were all these adjective descriptors. But no pictures, just this verbiage.
And then finally, if you just start tallying it up, there’s been over 1000 sightings of some kind of something in the Loch Ness.
Yeah, that’s a lot of sightings. And you might be wondering where are all the photographs. Well there are none. There is this one iconic one from 1934 that probably a lot of you have seen, we can bring it up. And this photo was proven to be a hoax in 1994. So for 60 years they thought this was an actual photograph.
And it still persists.
During that time there was speculation that maybe the monster was a Plesiosaur, which is an ancient marine reptile. But paleontologists have pointed out that the Loch was frozen until about 10,000 years ago, and a cold-blooded reptile would not be able to survive the frigid temperatures.
So what are some other theories to explain what over 1000 people are seeing? I know one has to do with eels.
Yeah, eel. They can be a few inches, they can be a few feet, and I guess some of the bigger ones in the world can be close to 12 feet. And they’re kind of snake-like and they have double sets of teeth, so they’re quite a creature.
There were people who got a lot of – there were surveys, analysis done of DNA in the lake, and they found a lot of eel DNA. So that was these moving creatures I mentioned, all around you every stroke. A water skier never falls. Maybe they didn’t water ski back then, I don’t know.
Big trees, they can get heavy and sink to the bottom, and they can become water-logged and they trap air. And sometimes they’ll refloat and then during storms they can be tossed about, and maybe somebody filmed a big tree being lurched up in the air during a massive storm; I don’t know.
And then the Norwegians decided to do a little more work. They were combing along on the bottom of the lake, and they found what was kind of initially interesting but it turned out to be a movie set that during the filming of The Private Life of Sherlock Holmes, this whole set settled down and fell into the bottom of the lake. So the Norwegians were finding an old movie set.
That was from 1970, so that doesn’t actually explain earlier sightings.
No.
Okay, so apparently in 1987 they decided enough was enough, and that they were going to find out what was really in the Loch, and they launched Operation Deepscan. And this was an international team with over a million dollars of high-tech equipment, they lined up 24 boats to span the loch, and each had cutting edge sonar that case a wall of sound down to the deepest parts of the loch, and for over a week they traveled this 23-mile length. They did not find a monster, but they did pick up on three sonar contacts that indicated quote “something big.” So the bottom line was that the results were inconclusive. They couldn’t prove that there was a monster, but they also couldn’t prove that there wasn’t.
So I guess the BBC’s Clyde Ferguson said, “If nothing else, Operation Deepscan has proved one thing: you cannot kill a legend with science.”
Kind of reminds me of endodontics in the literature. You can believe whatever you want to believe, read whatever you want to believe, quote whoever you want to quote. But people do have various interpretations of all this, and it’s interesting to hear with so little evidence, almost no photographs or zero photographs, it does live on very strongly.
So my only comment in the closing for me would be, be very careful when you open up the mouth and you go inside, because every mouth could hold its own endodontic, monster tooth.
Yes, some mystery there for sure. Well that’s our show for today. We hope you enjoyed it and we’ll see you next time on The Ruddle Show.