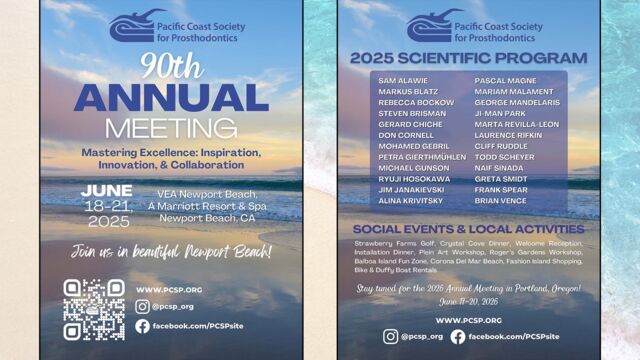
Pacific Coast Society for Prosthodontics: 90th Annual Meeting (informational graphic) - Courtesy of PCSP
The Endo-Antral Connection Special Guest Presentation by Dr. Roderick Tataryn
The show begins with a little promotion of an upcoming dental meeting by the Pacific Coast Society for Prosthodontics. Guess what? Ruddle will be speaking there! Then, Dr. Rod Tataryn gives a presentation on better understanding the role of endodontic infections in maxillary sinus disease. After, Ruddle and Lisette share insights in a post-presentation discussion, highlighting some key concepts. The episode concludes with a Ruddle case report that is representative of the kinds of cases he plans to show at the PCSP meeting in June.
Show Content & Timecodes
00:38 - INTRO: Pacific Coast Society for Prosthodontists – Annual Meeting 05:26 - SEGMENT 1: Guest Presentation by Dr. Roderick Tataryn 42:29 - SEGMENT 2: Post-Presentation Discussion 54:48 - CLOSE: Case Report – Endo/ProsthExtra content referenced within show:
- Special Guest: Dr. Roderick W. Tataryn
- Dr. Rod Tataryn’s Professional Practice: www.drtataryn.com
- Pacific Coast Society for Prosthodontics 90th Annual Meeting, June 18-21, 2025; Newport Beach, California: www.pcsp.org (see also downloadable PDF below)
- Dr. Cliff Ruddle PCSP Lecture Graphic (see downloadable PDF below)
- Dr. Terry Pannkuk, Pure Dental Learning: www.puredentallearning.com
- Tataryn RW, et al: Maxillary Sinusitis of Endodontic Origin: AAE Position Statement, AAE, April 2018, https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/04/AAE_PositionStatement_MaxillarySinusitis.pdf
- Stropko JJ: Canal morphology of maxillary molars: clinical observations of canal configurations, J Endod 25:6, pp. 446-450, 1999
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al: Clinical Practice Guideline (Update): Adult Sinusitis, OTO Journal 152:S1-S39, 2015, https://aao-hnsfjournals.onlinelibrary.wiley.com/doi/epdf/10.1177/0194599815572097
- Ingle JI, Rotstein I: Ingle’s Endodontics (Volumes 1/2). North Carolina: PMPH-USA, 2019
‘Ruddle Show’ episodes & podcasts referenced within this episode:
- Find referenced shows within the You May Like tab above
Downloadable PDFs & Related Materials
Ruddle Lecture Slide - "The Endodontic View: Through the Ruddle Prism" (as part of his lecture for the PCSP 90th Annual Meeting)
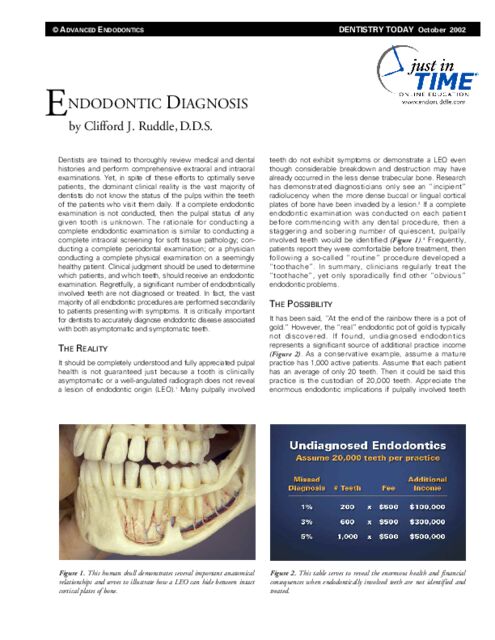
Dentists are trained to thoroughly review medical and dental histories and perform comprehensive extraoral and intraoral examinations. Yet, in spite of these efforts to optimally serve patients, the dominant clinical reality is...
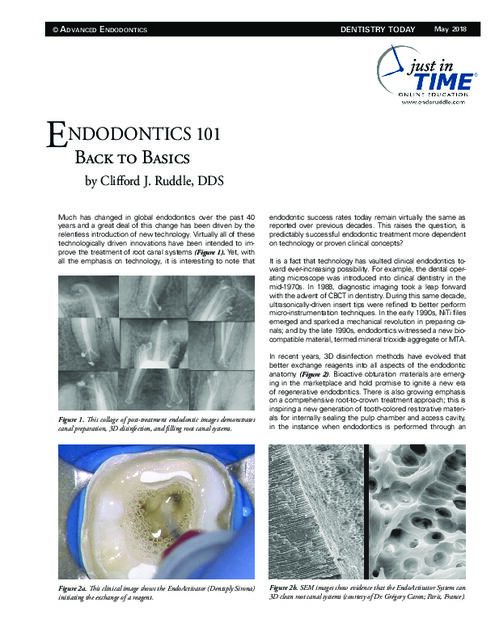
Much has changed in global endodontics over the past 40 years and a great deal of this change has been driven by the relentless introduction of new technology...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
OPENER
…Clear!... [airplane engine starts]
INTRO: Pacific Coast Society for Prosthodontists – Annual Meeting
Welcome to The Ruddle Show. I'm Lisette, and this is my dad, Cliff Ruddle.
How are you doing today?
Pretty good. How about you?
I'm doing excellent. And I want to welcome everybody out there. You're--if you're counting, we're in season 12 and we're in show three. So, three of 10, here we go.
Okay. Well, we wanted to take a moment at the start of this show to talk about an upcoming meeting by the Pacific Coast Society for Prosthodontics. You can see behind me and it's going to be June 18 to 21 in Newport Beach. And it's their 90th annual meeting and scientific session. So, also, you will be one of the speakers there. So, we'll talk about what you're going to be lecturing on in a second, but first why don't we bring up the meeting flyer that shows all the speakers' names on it. So, first why don't you maybe just highlight in general some things about this meeting?
Well, the meeting promises to be fabulous because if you see all those speakers, all of them have something to say each in their own way, and it'll be intended to forward our education and learning. So, just in a matter of a few days, you're going to see a lot of people. And I'm pretty excited about it. Jean Wu, Dr. Jean Wu, a prosthodontist, she's in the Paquette Cheryl Sheets office. We've spoken about them many times. And Cheryl's been on the show. This is her partner, Jean Wu. She's going to be on the Ruddle Show later this season, but she's also the planning organizer of the meeting.
So, my invitation came from Jean Wu. I want to acknowledge her and it's not such a bad place to visit. It's a very beautiful setting. I don't golf, but they're going to play golf and tennis and do everything. It's going to be marvelous. And finally, get to see a lot of friends, maybe meet some new friends and it'll be fun.
Yeah, it sounds like it might be a good place to bring the whole family, too.
That's what she said happens. A lot of families do come.
Okay. Well, just looking at this list of names, they're all great speakers and leaders in the profession. Is there anyone in particular that stands out to you that you're really curious to hear what they have to say?
Well, I'm really curious about several of them. I actually have penciled in a couple that I plan to go to their presentations. One's going to be Frank Spear. Frank Spear is giving something about lessons learned in 40-plus years of doing prosthodontics. Frank was on our Legacy Show for 100 last season. He's a longtime friend and a fabulous speaker. You'll learn a lot. So, I penciled him in. And then, Pascal Magne, he's a fabulous clinician and he's a teacher and he's got Magne education, textbooks, videos. He is an artist and I just admire his attention to detail. Then finally there's Gerard Chiche. He's from the Georgia Regents University School of Dental Medicine. He is the Chair and he runs the program of Aesthetic Dentistry and Implants. So, he's doing 45 years.
Yeah, I see it as a 45 year perspective. And I think Frank Spears’ was 40 plus years.
40 plus.
A lot of experience there.
I like that because she just said it. You know, you can go see somebody that's 35 years old and you're going to learn something because they all probably have something brand new. But I also like to see what works and the mistakes that were made, the adjustments that were put into place, like a structure to address that, and how the cases keep rolling along. That'll be fascinating.
Okay. Well, we just mentioned that there was going to be a lot of experience there, but they also have a graduate prosthodontist student research competition.
They do.
So, I always like it when they have stuff like that. All right. So, let's talk now about your lecture and let's bring up your lecture slide.
Oh.
What is your lecture gonna be on?
It's the endodontic view through the retinal prism. You see, I have a special way I look at things. And so, I'm gonna share that with the group. But a lot of times in interdisciplinary treatment--well, I don't really have anything built besides that. I mean, that's--I'm going to go with this title slide for my 40 minutes. The longest speaker—
Well, this title slide really nails it. It's really very Pink Floyd, Dark Side of the Moon.
So, you can see how the runner, you know, he looks in there and it goes this way and there's rays of light going all places. Anyway. I haven't got anything else than this, but maybe with some time, I'll get a presentation together. Anyway.
Okay. Well, at the end of our show today, you're going to show a case report that is representative of the kinds of cases one would expect to see if they come to your lecture. So, we'll see that at the end of the show today and look forward to that. But first, we have actually a special guest presentation today. So, let's get to that.
SEGMENT 1: Guest Presentation by Dr. Roderick Tataryn
Okay. So, today we have a guest presentation, which you will see momentarily. It is by Dr. Roderick W. Tataryn, who is an endodontist from Spokane, Washington. And he has become a leader in understanding the connection between endodontic infection and sinus maxillary disease.
He has.
And in fact, that's going to be the topic of the presentation, which is called the Endo-Antral Connection. But before we watch it, why don't you tell us how you know Dr. Tataryn and how it came about that we have the opportunity to show this presentation today?
Well, according to him, when we were talking by Zoom, we had a very nice talk about the show. I said, have I physically met you? Because I've read a lot of your articles. He’s in, I think five textbooks and stuff like that. Anyway. He said well, when I was at Loma Linda University as a resident, he said you used to come down there when Leif Bachman and Mahmoud Torabinejad were sequential chairs. And he said, we saw you quite a bit. And he said, you actually inspired me to be an endodontist. So, that was nice of him.
And anyway, he said he's seen me here and there, but he might have been a face in the crowd. But I'm delighted to have him on. I got his name from Terry Pannkuk, your endodontist. And Terry had him on Pure Dental Learning. That's Terry's website where he does his education. So, Rod gave a much longer presentation than he was restricted to about, we told him 20 or 25 minutes. So, he was restricted in time. Terry let him go crazy. So anyway, Terry, I trust, Terry's been on our show, so Terry said Rod gives a wonderful presentation on lesions of endodontic origin and how they affect the maxillary sinus.
The other thing to say about him before we go further is Google his office, he has a tremendous office. What you're noticing is clean, neat, modern. You're noticing technology, you're noticing staff and grooming and just all the things that comprise excellence. So, that would be worth doing. We might have some pictures we can drop in.
And then, I want to talk about a little hobby that almost none of them would know he does, but he's quite a pilot and he's a pilot of old planes, like from the 40s and 50s. So, currently he's rebuilding--he's just finishing rebuilding a 1942 Ryan PT-22. And that plane, just so you'll know, cause I didn't know, he just told me it was that plane. So, I Googled it, but that's what the U.S. Army Air Corps instituted just around World War II, because that was a first model plane frame where they taught pilots that were going to go to Europe and drop real bombs.
So, anyway, he said it has--it's ‘42, but it hasn't been flown since 1956. So, he--we'll have some footage a little bit later.
I think we actually have some footage right now to show off him starting up the plane.
Oh, that's the best part.
[Airplane video plays]
Do you want to fly with him?
Okay. Well, just to tell you a little bit about Dr. Tataryn professionally, he earned his DDS degree in 1989 and his Master of Science degree in 1994, both from Loma Linda University, where he maintains a faculty position. He has also served on the Clinical Practice Committee for the AAE and he is currently a reviewer for the JOE. In addition to maintaining a private practice for more than 30 years, he lectures internationally. He has published numerous articles, clinical articles and scientific papers on endodontics. And he has also contributed to five endodontic textbooks, including Ingle's 6th and 7th edition, and also the Art and Science of Contemporary Surgical Endodontics. So, that's-
I want to add one thing. It's really interesting that he is in the books that we both have chapters in.
Yes.
And the cover of that book, he doesn't even know it, so I'm telling him because I know he's going to watch this. On the cover is a maxillary molar. So, Ron, I put that maxillary molar, my team gave that to the Ingle textbook, it's on there to remind you of the maxillary sinus.
Okay. So, we're actually very honored to have the opportunity to show you this presentation, so let's see it.
[Tataryn Presentation Begins]
Thank you, Cliff, for inviting me to present on The Ruddle Show. It is a true honor to be here. Cliff, you've been a mentor to me my entire career, graduating as a general dentist in 1989, practicing general dentistry for three years, Palm Springs, listening to everything you said and wrote. Big encouragement for me to go into Endo. Thank you. Endo at Loma Linda. Of course, you were on faculty as a lecturer at Loma Linda. You came out and spoke with us as residents back in ‘92 or ‘93 and great influence on me my entire career, Cliff, so thank you. It's an honor to be here on your Ruddle Show and your current program.
This is a subject that's near and dear to my heart the Endo-Antral Connection. It's a topic that's had a lot of great increase in increased attention in the last probably five years in the literature, and it's gaining some momentum. It's still a little underappreciated in, not only among general dental practitioners and even some endodontists, but we've got to get more word out to ENT physicians, radiologists, and mainly the coordination between the dental community and the ENT community still has quite a bit to be desired.
As we all know, the maxillary posterior teeth protrude into the maxillary sinuses. In many cases, these highly pneumatized sinuses really become a communication between the root apices and the floor of the sinus. In fact, in this 3D rendering, we see that the roots are essentially forming the floor of the sinus here in the molars. About a third of cases will have the roots protruding up and the sinus dipping down between the roots of maxillary molars. Over on the left here we have a sagittal CT--sinus CT image, and you can see the same thing, roots protruding in.
So, ENTs know this, general dentists, endodontists, we all know that this occurs. Of course, if there's an endodontic infection, it's very easy for that infection to progress into the sinuses rather than into the oral cavity. In most cases when we have a periapical infection, apical periodontitis and acute apical abscess, we can see that radiographically with missing bone and with damaged cortical plate. We can develop sinus tract stoma or in this case an intraoral or extraoral swelling. If that broke lingually, we could get a submandibular sublingual swelling. Either way, it's going to be noticeable clinically with patient having symptoms, pain, visible signs, and of course very evident radiographic issues--findings.
And we can see that when we treat an endodontic case properly and manage it appropriately, we can expect healing within six months to a year. We should expect full bone resolution, which can also be seen very evident radiographically.
It's a little different when we're dealing with teeth, the maxillary posterior teeth and teeth near the sinus. In this case, we have an upper bicuspid with a necrotic pulp, paraplegic lesion breaking through the cortical plate and developing some intraoral signs. So, it'll either be a sinus tract stoma here, a little fistula, or intraoral palpation tenderness or even swelling. All this is going intraoral because it's gone through the buccal cortical plate. It's also very visible radiographically because when we break that cortical plate and have that radiolucency, it shows up very well on a periapical film.
However, if we have the same infection that happens to break lingually or anteriorally and keeps the cortical plate intact on the buccal side, that will block our radiographic view, making it very difficult to see on a radiograph. It'll also have lack of all intraoral symptoms. There'll be no sinus tract stoma, no swelling, no infections getting into the oral cavity. So, it'll be easily missed in a dental clinical exam visit. Patient symptoms in this case will be typically anterior. They'll have mucosal swelling and if this goes acute and that instead of having an intraoral or extra oral facial swelling, the sinus will fill with that pus and it will obstruct the sinus entirely and even progress further.
This is a view radiographically. This is a slight periapical osteoperiostitis. We're going to explain that in a minute here, but this is an expansion of the periosteum. It's very faint on periapical films. It's very hard to see if there's any dental infection because we really don't see sinus obstruction. We've got a cheekbone in the way. This is the problem with periapical views.
This case went to an ENT first because the symptoms were not dental. They were cyanogenic. And there's our lesion, our radiographic lesion on CT. Fully obstructed sinus in this case. This is the coronal view of that same case, and it has progressed not only via the maxillary sinus, but into the ethmoids, and has caused pus to flow into the nasal cavity via the ostium. This is a middle turbinate. We're gonna explain a little of this anatomy in a minute here. And the pus comes just behind that middle turbinate out the ostium, and that's what the ENT sees when they scope a case like this. And all the while, the patient has no dental symptoms, no findings, and they pass their last recent dental exam with flying colors.
So, this is the problem we are facing, and this is what we want to discuss. How common is this condition we call odontogenic sinusitis? It's very common. About 40% of chronic rhinosinusitis cases will have a dental source or cause for it. Over 70% of those will show up if they're unilateral sinus infections. I should say 70% of unilateral sinus infections will have a dental cause.
So, recognize that this is a very common issue. Of course, this is all dental-caused sinus issues. Odontogenic sinusitis is a very broad term. This pathologic extension of dental infection into the sinus that will be symptomatic or cause typically some sinusitis symptoms or obstruction. It's also called MSDO or maxillary sinusitis of dental origin and a few other names. Again, it's a broad term. It refers to all dental causes or etiologies, endodontic, periodontal, extractions, dental implants. When I say extractions, I'm talking about potential oral-natural communication or fistula that develops, or the foreign body of a tooth actually going into the sinus.
Dental implants, again, often implicated in odontogenic sinusitis. Root fractures, great pathway for bacteria up the root into the sinus. Again, iatrogenic causes, extruded dental materials, displaced teeth, foreign bodies. These are all causes of odontogenic sinusitis. But MSEO is specifically the extension of endodontic disease, apical periodontitis, into the sinuses. This is the number one cause of ODS, or odontogenic sinusitis. Probably 40% of ODS is endodontic, or what we call MSEO.
And so again, that's specifically induced by endodontic etiology. It was very important that this term was defined because everything was getting lumped together in the same umbrella of ODS when the majority of it's endodontic. They're all different etiologies and they all have different treatments, so we needed to separate this out. So, we termed this coin MSEO in 2018 via a position paper that a group of colleagues from the AAE and I, who were on a special committee, formed and wrote this paper that was distributed to all the ENTs in the US as well as endodontists. And it's available on the AAE site. So, it'll dovetail well into this lecture. So I encourage everybody to go on the AAE website and download that and read it.
But defining it specifically, this is the periapical lesions that have progressed in, they're creating a little bit of inflammation. But if that's left untreated, you'll have that same case. Go into a full sinus obstruction. Of course, that can progress even further up into the ethmoids as we saw in that previous case. Remember, these are unilateral typically. There's our lesion. There's a full obstruction. Here's another side, another lesion causing sinusitis. These are all MSEL, endodontic-induced ODS. And you'll notice that again, they're all unilateral or one-sided. They're all on the same side as the source of the infection, of course.
So, I think it's really important for us to just kind of, especially depending on the audience that's listening to this, kind of a quick overview of the anatomy. All of us should be—it should be incumbent upon anybody that treats our patient in the dental field to understand the anatomy of the sinuses because this is where our dental infection often goes. This is the pathway it often takes.
So, we have four pairs of paranasal sinuses. The maxillary sinuses are in purple here. They're the largest of the sinuses. In blue, we have the ethmoids. Frontal sinuses are in green. Sphenoid sinuses are in red. Again, the most prone to infection are these maxillary sinuses. Why do we have them? What's the purpose of sinuses? Well, they produce mucus. Their number one goal is immune defense. So, they're producing mucus a liter a day in the average adult, two liters in a diseased state.
Again, it's immune defense. There's antibodies and antibacterial proteins in that mucus. It traps, it filters particles, dust spores, bacteria. Moves them out of our sinuses and prevents us from breathing them in. And then, gets them down into the throat where they're swallowed and digested. So, it humidifies, it warms the inspired air. The spaces are also thermal insulators for our eyes and for our brain. Sinuses give our voice resonance, tonal quality. The different shapes and sizes of sinuses give us all our unique sound. They reduce the weight of the skull. They absorb impact in a trauma.
So. there's a lot of reasons why we have sinuses, but again, number one, immune defense, producing mucus. So, let's talk about that organ that produces that mucus and moves it. This is the bone that overlies the sinus. Overlying that bone is periosteum. And then, in between the mucosa and the periosteum is this layer called the lamina propria, and that's this loose connective tissue that forms or harbors the blood supply that feeds all this immune defense.
So, we have a lot of blood vessels running through that lamina propria, all held together by loose connective tissue. Above that, of course, is the pseudostratified columnar epithelium. That is the epithelial layer that houses these little goblet cells and these mucus-producing glands that are a little larger. They all produce, again, lots of mucus, little ciliated cells that move that mucus all in kind of a singular direction. And the direction of that mucus flow is up—these are the cilia here in an electron microscope view—but they move that mucus in a singular direction, and that's up toward the ostium where they're draining and draining to the nasal cavity.
Here's the frontal sinuses draining out, the ethmoids all draining into this same area here we call the ostiomeatal complex, and that's right behind the middle turbinate in the nasal cavity. And that's where we saw that pus coming out on that one image. So, we see a very evident path or flow of mucus all into the nasal cavity again, where it's swallowed and dissolved by digestive acids. Here's that mucus coming out, the maxillary sinus ostium. This has been surgically opened, but still nice flowing mucus behind the middle turbinate MT over here.
What is rhinosinusitis? How does that differ from ODS? Well, rhinosinusitis is an obstruction of the ostium. That is the center key area where rhinosinusitis develops, and it is basically an obstruction of that ostium. It's obstructed either via an allergen or a virus or a bacteria. There can be an anatomic obstruction as well—septal deviations or dried mucus or polyps or anything can block that and cause inflammation and mucus buildup within a sinus.
The symptoms that a patient feels when they develop rhinosinusitis are typically facial pain and pressure, some feeling of congestion in their cheek, below their eye. Nasal obstruction is in about 50% of the cases. A lot of times they'll breathe just fine through their nose, but have pressure in the cheek or below their eye. Post-nasal drip is common. Altered sense of smell is common as well. Fever occasionally. Headache, one of the minor symptoms. Bad breath. Fatigue. Dental pain. Again, dental pain just because those teeth are protruding into the sinus. They can be perfectly healthy teeth, but feel aching and pain from pressure in the sinus. Patients can have a cough, ear pain and pressure. Again, minor symptoms.
But these are the symptoms a patient may experience when those sinuses build pressure from obstructed osteo, from the symptoms of rhinosinusitis, and that is bilateral, usually both sides in a chronic rhinosinusitis. What do ENTs do to manage or treat rhinosinusitis? First thing they do is antibiotics, typically. First line, amoxicillin, doxycycline, that's usually a general physician, GP, primary care guy will give that. Once they go to the ENT, they're going to be up to Augmentin or the quinolones such as Cipro or Tequin and Levaquin, those things. Often, Flagyl, Metronidazole, and Penicillin or some of the cephalosporins or clindamycin.
These are all some of the similar antibiotics we'll use for anaerobes in dental infections, same thing. Adjunctive treatments after antibiotics, they'll also encourage saline irrigation, maybe topical steroid. And if the patient's not getting relief from those things, they'll step up and do functional endoscopic sinus surgery. And these are typically done outpatient, where they'll open up the natural ostium, get some drainage.
What that looks like is there's an uncinate process right here, separating the maxillary sinus and there's if you would take cuts further back, you'd see that that would open up if it's not obstructed. Well, they just remove that entire uncinated process. Just open that up. It's called a middle meatal antrostomy or an uncinectomy. So, these are what the clinical practice guidelines recommend for treatment of maxillary sinusitis. And the patients or ENTs that follow these guidelines will follow this method of antibiotics, adjunctive treatments, surgery if that doesn't work.
What's missing from the clinical practice guidelines is any mention of an odontogenic cause for sinusitis. So, ENTs typically aren't really looking for that because there's just no recommendations in the guidelines for a dental exam or an endodontic exam specifically to look for a dental source. So, often these cases get treated with sinus surgeries that are actually odontogenic sinusitis, not rhinogenic sinusitis as they were diagnosed as.
And as we see, opening up the uncinate process there, the natural ostium, widening it and opening it, will still leave continued infection on the floor of the sinus even though it has a bigger pathway to get out into the nasal cavity. Here, the ethmoids were opened up, even had a partial turbinectomy done here, and just to really open this guy up, but yet persistent sinus infection, foul odor, drainage, all unilateral, classic signs of MSEO or endodontic ODS that was mismanaged by ENT surgery, otolaryngologic surgery.
So, we really need to understand that MSEO, this endodontic cause for sinusitis, is going to end up first at the ENT's office because the dental symptoms just don't show up. They're not present. The thermal pain is absent because we're dealing with necrotic teeth that have apical lesions or failing endodontic treatments. Previous root canal therapy mostly missed canal systems. Percussion tenderness isn't there because they're not building up any pressure in bone, and we're not going to see any inter-oral swelling or any inter-oral findings again as we showed in those earlier films.
Patients are typically going to have sinonasal symptoms, all those symptoms of chronic rhinosinusitis, you know, building up of pressure in the sinus. They're gonna have foul odor. They're gonna have maybe some postnasal drip. And again, they're gonna be unilateral, but they're gonna end up going to their ENT first with those feelings of congestion and facial pain.
And so, this is how these things often get missed. We have a real limitation, as we mentioned earlier, periapical radiographs just not showing this stuff. They will vaguely show them, but they're a two-dimensional image of a three-dimensional object, right? So, they're subject to all kinds of interpretation errors. We have elongation and foreshortening problems. We've got superimposition of the cheekbone and the palate and the sinus, and everything's kind of in our way when we look through a periapical film radiograph. And it just won't ever show any soft tissue or sinus mucosal swelling or fluid in the sinus. Those are very hard to read on periapical films.
So, cone beam CT really is our gold standard for management and diagnosis, I should say, of MSEO. Here's a great example of a cheekbone just blocking our apices, not able to really make out is there a lesion here on this tooth, is this something? But once we go to an ENT, we can tell, yeah, there is an MB lesion, but look at the big lesion over the second molar that is just really very vague on a radiograph. There's a little evidence of that periostitis, that inflamed halo or periosteum.
And then, of course, all that mucosal tissue, can you really make any of that out? You kind of could if you squint, but the scan just takes it and makes that just so obvious. We can look at that coronal view, see it breaking through the periosteum into the sinus here with mucosal tissue and green arrows. There's that missed MB2 on the first molar causing that mesial lesion on this one, which again with time probably will also progress into the sinus.
So, armed with that kind of information, we can get after these teeth, we know the anatomy, we can get in and find the MB2, we can disinfect, clean, and get these things healing and get these patients healthy and prevent them from developing a full-blown odontogenic sinusitis of endodontic origin there. We need to define some terms. Periapical osteoperiostitis, which I mentioned earlier, that is just an expansion of the sinus floor periosteum. Remember that lowest level of that tissue example I showed? That's those structures, the lowest level, the lining of the bone, periosteum, expands in the presence of inflammation. That inflammation and pushing up of the periosteum will create a periosteal reaction, what we call a reactive osteogenesis.
New bone will form on the floor, on the inner periphery of that periosteum, which is the cambium level or layer, and that makes new bone, creates a little halo or a radiopaque dense expansion, which is really nice for endodontic diagnosis. And it can really expand very large in some of these cases. Oftentimes they're asymptomatic, they don't have to have any symptoms whatsoever.
Here's an example of periapical osteoperiostitis, that expansion and that new layer of bone that forms on the inner periphery of the periosteum. Creates a nice halo, makes it really easy to see. Of course, once the endodontic treatment is done, that bone goes right back to normal and the sinus floor goes back to its previous dimensions.
Something happens when that periosteum gets perforated and that's the mucosa can swell up. Pericopic mucositis is the term we use for that, where the infection really perforates or breaks through. And you can have pericopic mucositis even in cases combined with some osteoporosis. But it's basically defined as just an edema or swelling of that mucosal tissue of the sinus or mucosa.
So, this is characterized again by thickened mucosa. I can have different variations. It'd be kind of dome shaped. It could kind of look like, you know, bumpy. It can have more of a mucosal thickening that is just sort of more generalized over the floor. But you can have that without any osseous damage evident at all or any expansion of the periosteum. The problem is it's very similar to a mucous retention cyst or any other mucosal thickening that can happen for a number of reasons.
So, it's very difficult to say, yeah, that's for sure tooth caused. But if you see an expansion of that sinus mucosa right over a potentially infected tooth, it's really important to just check the tooth for necrosis or failing root canal therapy because that mucosal inflammation can expand and become a complete sinus obstruction and then travel further into other areas, other sinuses, and even worse. So, and we'll show that coming up.
Periapical mucositis is an example of that. Here's an untreated lingual canal in a first bicuspid, well-treated buccal canal, but when we look at it from the lingual or the sagittal point of view so we can see that untreated lingual or the axial view we can see an untreated lingual. It's perforated a hole in the sinus. It hasn't really expanded the periosteum. There's really no halo there at all, but we see that thickened mucosa. That's periapical mucositis and here's our perforation of the sinus floor.
Treating that untreated lingual canal, six month recall or seeing the sinus completely cleared out, that'll clear out, that periapical mucositis will probably clear in about two weeks. Certainly, inside of a month, it should be pretty much back to normal. And then, we have a little bit of healing to go here on the bone at six months. But we can expect real easy, quick resolution of the mucositis with endodontic treatment. If that is left untreated, it can progress, as we said. It progresses all the way to a full sinus obstruction up into the ethmoids.
In this case, it actually perforated my patient. This guy came in to me from his ENT, who sent me these images, that perforated what we call the lamina propria, that's a thin little bone between the ethmoids and the orbit. It's the thinnest bone in the orbit, and it was causing an orbital cellulitis for this patient. As you can see, it's very vague. The radiologist did not pick up the dental lesion, it was the ENT that said, we need to check the teeth for this, even though the radiologist saw the pathway up in the eye. There was no mention of a dental infection that was evident. But he did notice that thinning of the lamina propria.
Let me show you what that is. This is the area in the orbit. It's the thinnest wall of the orbit. Again, it's called proria (phonetic). It's named after papyrus because it's paper thin. And it's very easy for a dental infection in the ethmoids or any infection in the ethmoids under pressure, to perforate into the orbit and cause an orbital cellulitis.
So, this was the patient right before we saw him for treatment. Here's that lesion. We went ahead and took our own cone beam. It's a little more evident on a cone beam CT than it was on the sinus CT. There's the perforation right below my picture here on the scan 3D. And we went ahead and treated him in two stages, did a calcium hydroxide interim medication, a month later came and obturated and filled those canals and had resolution, a lot of improvement. Of course, that was in conjunction with middle-meatal antrostomy, that uncinectomy to open up and drain the osteomyelitis complex.
I have—this is another case that was just sent to me a few weeks ago here by a colleague that I've co-written some papers with out of Detroit. He's at Henry Ford in Detroit. He runs the program, John Craig, over at Henry Ford. And this is a case that he had just seen late last year that progressed from a molar and a first molar mesial root, as well as the first bi, two infections, progressed. This is a little later, this is a previous film, but this is a little later in 2024, up through the ethmoids and into the brain. And then, of course, he had a cranial infection here that they had to open him up and drain all this subdural pus from. So, these--and there's plenty of case reports of these cranial infections from endodontic abscesses that progress through the sinus and up into the brain.
So, we've got to be really careful and cautious with our diagnosis, making sure that we're not missing this stuff in dental practice if at all possible. This is a patient that came to me from ENT. Again, full obstruction of the maxillary sinus, ethmoids, and up into the frontals, very close to an orbital cellulitis or brain abscess. And so, the ENT and the radiologist both picked up these lesions on the upper first molar, sent the case to me. We went ahead and treated it.
This is our cone beam CT, again, very evident, full obstruction. Went ahead and treated this case. Everybody followed the case. They had a surgery by the ENT to open up and drain everything. It's essentially an IND that we would do for an acute abscess intra-orally, but they're just doing it nasally, intranasally, by opening up that ultimate process, getting all that pus out. And following treatment, following their surgery combined, we have a full resolution of the sinusitis.
So, another note to make to anybody treating or doing endodontics in these upper molars, realize the MB2 is a thing. It's there. It's a common issue. It's critically important that we manage and treat MB2s, especially because many of them have their own separate orifice. Missing one canal in a four canal tooth is absolutely no different than missing one canal in a one canal tooth. You didn't do the endo. And lesions can persist, causing MSEO, and then causing a full-blown emergency for the patient in their sinuses.
What is the incidence of MB2? How many times can we expect to find this? John Stropko did a great clinical observation study in his own practice. Once he brought the clinical microscope out, he was finding MB2s in maxillary first molars at a 93% find rate. His second molars, he was finding them at a 60% rate. Phenomenal treatment. John's a great endodontist. I can't attest that I'm quite that high, but I aim to be that high. That's what we should be getting.
Karabucak had a study in JOE in 2016, finding that the incidence of untreated canals was extremely high. He reviewed 1,397 CBC, almost 1,400 cone beams, and he found that 23% of endodontic cases had missed canals. The majority of them were maxillary molars, 40% of endodontic cases had missed canals. The majority of them were maxillary molars, 40% of them, and the majority of those, the highest number was the first molars, teeth numbers 3 and 14. Again, missed MB2s, the absolute number one missed canal in all of endodontics. And these teeth with missed canals, over four times more likely to be associated with an infection.
I can't stress enough the necessity for the use of the surgical operating microscope in the treatment of maxillary molars. Really, it should be used for any case at all. But being that the maxillary first molars are the number one missed canal tooth, none of us should be even thinking about performing endodontics on maxillary molars without an operating microscope or referring to someone who does use one. Finding MB2s, getting all the anatomy, disinfecting, thoroughly treating these cases is what's going to be necessary not just in healing endodontic disease, but in preventing MSEO and some very serious infections for others.
So, we're running out of time. Just a quick shout-out here to Ingle’s Endodontics 7. If you want to read more on this subject, I have a chapter on that. I actually have a chapter on Ingle’s 6 as well, but that's a little dated now. This is the most recent Ingle’s. Also, if anybody wants further reading or a pamphlet that they could hand out to colleagues, the AAE has Maxillary Sinusitis of Endodontic Origin that I wrote back in 2018. Very good research, very good references in that. Again, getting a little dated now. We should probably update a few things, but very good information for you to pass along to others.
Again, thank you very much, Cliff, for this kind invitation to speak to your distinguished audience, and hopefully this was some good information for everyone. So, appreciate you, Cliff. We will talk soon, my friend. Take care. Bye.
SEGMENT 2: Post-Presentation Discussion
Okay. That was an excellent presentation. Very informative. I learned a lot and it also was very organized. I do think though that it was maybe one of the scariest presentations we've had because being someone who has a lot of allergies and sinus issues, I immediately went down the rabbit hole and I already thought I must need many root canals. I probably had infected sinuses and that infection was well on its way to my brain. So, after I took a good night's rest, in the morning, I felt fine. And so, I'm now moving on from that. But I thought it was a great presentation. What about you?
It was absolutely awesome. I say awesome not very often about different people or even thinking something I did was pretty good, because we've heard all these things over the years from so many, and what Rod did is he took a topic that is really not discussed much, certainly in our field, dentistry. I mean, there's some discussion, but it might be like, what, five minutes in four years? So, I thought he hit a topic that was relevant, timely. I thought it was very appropriate, and I thought it was really a clarion cry to become better diagnosticians for physicians and dentists alike.
Yeah, you--well we'll get to that later, but I think he did say that 40% of sinus infections have a dental cause. And if you have a unilateral block, it can be up to 70% of the time that it's related to a dental issue. So, I thought that was kind of surprising, especially when he said that ENTs are generally not looking for dental issues, that that's not really in their guidelines or protocol.
Well, one of the reasons I liked his presentation and invited him, as Terry Pannkuk suggested, it was my own experience in the late 70s. And in the late 70s, you know, I was making relationships, having started to practice in the last five years, I was making relationships with periodontist, orthodontist, bachelor facial, and I decided I'm going to call a couple ENT guys and just tell them who I am. I'm an endodontist and we have a lot of endodontic infections that relate to sinuses.
And to make a long story short, over the next few years we shared many, many cases together. ENT was referring to me and I was referring to ENT. Finally they said, get down here, come to Cottage Hospital here in Santa Barbara and see what we're seeing. And I finally just said, you know, well, you do the ENT, you guys are specialists. I'll be the endodontist. I trust you guys, but thanks a lot.
Well, with a little bit more persuasion, I did go down and I scrubbed in and they were showing me the sinus from their perspective. They made a hole the size of a dime over the canine and that's called the Caldwell LUT. They went in and stripped out the Schneiderian membrane and when they said look in, you could see maxillary roots with globs of granulomas tissue around the roots and they were saying, Cliff, that was an endodontic problem not a sinus problem and how come you're blah, blah, blah.
So, anyway I learned a lot about that in the 70s and so it stuck with me through the 80s, 90s, and up to now. And so, when Rod mentions this, these numbers you just reported; it's normal. For me, it's normal, and it's something that every dentist on the planet should be going like, I need to be more thorough. But Rod does make a kind of an indictment of physicians who are already physicians, but now they're in grad school and they're taking a residency in ENT. And he said, because he talks to a lot of physicians, he actually gives this lecture that we saw a glimpse of it. He gives that around the country with physicians, maybe two or three different physicians.
So, he's learned a lot about how they think, what they know, and who--the material they're subject to learn. They basically don't know any of that. And he said, basically when people come in with sinusitis, they usually go antibiotics. Okay? And then, he said, you know, if it is more persistent, they might change from like amoxicillin to Cleocin or something like that. He further went on to say, then if it gets a little worse, they might do some nasal rinses and some topical steroids, you know, all through the nostrils and up into the turbinates, etc. And then he said, finally, if that doesn't work, they will do a surgery procedure. So, that's kind of what their one, two, three is for people that present with sinus problems.
Yeah, I think that's a little concerning because he also mentioned that a lot of times those teeth may even be asymptomatic. So, you might not know that you have a tooth issue, that you need a root canal. You might think just as a patient that you just have a sinus problem if you don't have any tooth pain.
Absolutely.
You're not going to be going to the endodontist if you think you have a sinus issue. So, maybe how can a GP or an endodontist help with this issue?
I think the first thing starts with just training dentists right in dental school and certainly by the time, if we're saying endodontists in grad school, they should be baptized in this. There's an old expression I like to use in the practice, it's if you must speak, ask a question. So, when patients come in, we can have two scenarios. We can have a necrotic tooth. Well, we might want to know the diagnosis of the necrotic tooth, great, we're going to isolate and do a treatment, but we also want to study those roots carefully from different angles. Incidentally, the CBCT is the gold standard, as you saw in the lecture, but most of us don't have CBCT. Only about 5% do, so that means 95% are going to have to take three well-angulated radiographs. He mentions if you come too steep, you block things with the zygoma, the maxillary arch, the palate, the thickness of the buccal cortical plate.
So, a lot of things can kind of get lost. So, he said, be sure to ask questions. And you might not be able to see it is what I'm saying, but you might be able to hear the answers if you ask the questions. Do you have pressure unilateral, not bilateral? If it's bilateral, it's probably allergenicity. If it's unilateral, it's probably suborbital. Do you have pressure under your eye? Do you feel fullness in this? Does it feel like there's warmth or heat? Do you have postnasal drip? Do you have rhinitis or runny nose? Do you have--what else do you have? I have it in the notes, but, oh, depress the tongue. Be a physician. Depress the tongue and look in the oropharynx because we'll show on a future podcast some of the drains that you can see just by observation. Well, that should be a big warning to the diagnostician, the dentist, that they're dealing with a tooth that's not only necrotic, but there's a sinus overlay.
What else do I have here? And then the failing tooth. So, a lot of times you can be looking, looking, there's, again, they're not gonna have pain because it's fistulated. And when we have fistulas, people are asymptomatic. They might say, oh there's a paralysis, there's a bump, I see a little pimple or something. But basically, they can chew equally well left or right, they don't have any thermal sensitivity. And so, they're not coming in saying classic toothache.
So, we need to ask these questions. And then on teeth that are previously been treated, they could be failing. And the most common cause of a maxillary sinusitis with a failed little tooth would be the MB2.
Okay.
And we've talked about the MB2 on multiple shows, how to find it, where it is, frequency, incidence and all that.
Yeah. You did mention that we're going to talk about this more on an upcoming podcast, because when we were having a discussion about his presentation, we actually had--it just sparked so many ideas, that we're actually gonna do our next podcast on breaking this down into even more detail.
Thanks for the warning.
Yes. Okay. I do have a question. So, if you have a tooth that's hurting or you need a root canal and you also have a sinus issue, you have both.
Okay.
If you resolve the tooth problem, if you do a root canal, will that automatically resolve the sinus issue?
You know, almost virtually always, yes. So, she's saying there's a combined lesion. I'm going to say the etiology was endodontics. So, it's a lesion of endodontic origin, but it spilled over and became a secondary, like endo-perio, became a secondary sinus problem. Usually, if you do endodontics and you do it properly, you know, it's going to heal. They could be left with some allergenesis and some minor sinus issues, but more or less you'll take out that component.
Okay. So, maybe if it's a very bad sinus issue, you would refer them to an ENT also after you did the root canal, but maybe if it's just minor, you could have them back for a recall to see if it's kind of cleared itself up.
If you have, if you've done the treatment, of course, they walk out of the office and say goodbye, and you're laying an expectation that I think you'll see some improvement in your sinuses, but maybe not everything because we're not going to be able to address the allergenicity, if that is a component in your life. But recall is huge. You got to prep them for recall because when you have them come back, you want to see if there was lesions. Those lesions are responding, they're shrinking down, bone is growing in, healing is underway.
So, if they still had problems, then I would say, okay, we've ruled out endo and I even have evidence that the endodontic component is healing, whatever would be left, maybe should go back and we should revisit this with the ENT.
Okay. But then say you have a, I'm going to just take it a little step further. If you have a dual issue, just only handling the sinus part is not going to resolve the root canal part, right?
No--
It doesn’t work the other way.
That's a great question because that's kind of like selective treatment vital versus whatever initial treatment. That's another one of your brilliant things. You know, the sinus problem is not going to cause endodontic problem. I'll say that with total confidence. You can have roaring sinus, ethmoids, frontals, you know, we talked about sphenoid, everything. It can all be clogged up. You can lose your ostium. There's no more drainage, but it will not cause endodontic problems.
Now, you might have endodontics, your own daughter. I ran into her on one of my walks and she was saying, Papa, all my teeth hurt, they're all kind of achy. When I bite, it's just a little bit sore. And I said, is it one side? No, no, it's just one side, it's not both sides. And then she said, my sinus is really killing me. Well, I told her that the PSA, the superior alveolar, the posterior superior alveolar nerve runs in the floor of the sinus, so all the teeth that it feeds, those roots that approximate the sinus are gonna be sore. So, they'll be inflamed, but it'll go away as you take care of the sinus.
I think the brilliant part of the question was about 2%, up to 2% of the time when ENT goes in and cleans out the sinus through surgery procedures, they can devitalize a tooth. So, the incoming neurovascular components into the various roots of a molar, it can be amputated, it can be severed, it can be disrupted, and that tooth would become necrotic. So, sinusitis can cause a tooth problem secondary to surgery.
But it's pretty rare probably.
Pretty rare, up to 2%.
All right. Well, that's all we have time for right now. But a big thank you to Dr. Tataryn for that great presentation. Do you have any final comments?
Well, I really want to thank Rod. He's just a delightful guy and very proud of him. He's doing a lot of work and he's like a voice crying in the wilderness, but this seems to be one of his niches. And keep it going and maybe you'll encourage general dentists worldwide through your platform of going to over 100,000 general dentists, Rod. Maybe you'll be able to touch them and they'll start being better diagnosticians. So that was the clarion cry, be a better diagnostician. Thanks, Rod.
I just want to say one more thing. I really like what you said to maybe a call to action. Maybe, you know, get out in your community and meet some of the ENTs that you work with, introduce yourself, and, you know, just what were you saying that you did?
Because in life, as it is in practice, it's about relationships.
Okay. All right. Thank you very much. And that’s it for now.
CLOSE: Case Report – Endo/Prosth
So, this show has had quite a multidisciplinary feel to it. We had Dr. Tataryn show us the connection between endodontics and the sinuses. And at the start of the show we talked about the upcoming Pacific Coast Society for Prosthodontics meeting where you will be talking about the interrelationship between endodontics and prosthodontics.
Right.
So, now you're going to show us a case, and it's going to be representative of the kinds of cases you're going to show in your lecture. So, if you like these kinds of cases, you might want to attend the meeting because I think it's going to be well worth it. So, now I will step aside. You can show your case and break a leg, as they say in show business.
Okay. All right. So, during interdisciplinary treatment planning, oftentimes an endodontic examination will reveal teeth that are irreversibly inflamed, they're pulpless or necrotic, or teeth that have been previously treated endodontically and are failing. So, my goal in front of this group, this prestigious group of young prosthodontists, residents and dentists alike, is to basically show some methods and highlights that will reveal things in initial treatment, retreatment and microsurgical correction. My goals would be, if you were there, I would want to stimulate critical thinking, I would like to spark your imagination. I'd like to inspire inspiration.
So, let's look at a case. All right. So, here we have prosthetics. This is a classic four-unit bridge. It's pretty interesting to see that endo can be the foundation of periprosthetic. But if you look, the terminal molar, it would be a second molar. It's been treated endodontically by somebody somewhere at some time. You can see different eras of treatment as we have a silver point. Over here we have gutta percha and got silver point on the second bicuspid. And now the anterior abutment and the most venereal sense is now endodontically involved.
This case was from Southern California, south of Santa Barbara, about 100 miles. The endodontist that did this case made initial effort to get into this case, and you can see the access. If you kind of look at the crest of bone in here, and you look at the distance here, back to the crowns, and you look at the distance from the root, and you look up into here, you can begin to see it's about a little more than one to one. So, what I'm saying is in essence, this endodontist made a pretty good effort and weighing risk versus benefit, being that it's tied up into a four unit splint, we don't want perforations. We don't want to hollow out the tooth. We don't want to needlessly weaken the tooth. So, the idea was maybe I should stop, abort, fill the access cavity and go from there.
Well, he recommended surgery, but at some point, the patient was referred to Santa Barbara and that's how I got it. So, this is my pre-op. And so, when you're talking about endo-prosthetic cases, this would just be one, we're gonna show, you know, about 15 cases and then show about 15 in retreatment, about 15 in surgery to get to my 40 minutes. We decided to make a surgical approach. The lesion you're all pretty much noticing seems to be apical, and that would be probably a pretty good risk.
But if you look really carefully, and I didn't have CBCT then, but if you look carefully, you'll start to see, I'm kind of mapping what I see, I'm close to the board, but that's pretty dark in there. And I'll get these lines out. So, I think we have an apical lesion. I'm further thinking we have a lateral lesion because when I palpate, not apically in the fornix of the vestibule, but about mid-root, it's tender. So, I'm thinking maybe that is something in fact.
So, I'll just show you quickly now the procedures. I'm not going to make you surgeons, but the idea to this group, the PCSP group, is to show them what endodontics can do and how it can salvage cases that would be very disruptive if we lost the dentistry. So, I laid a flap, about a three-tooth flap, reflected the flap, and I cleaned out just some granuloma tissue. You see the granulomas tissues removed, and you can kind of get a sense that there's a root in here, and you probably see there's probably a root there. That's because we kind of see a root over here, and then we see a root like that. Also, you see right here a significant lateral portal of exit.
So, this is actually breakdown products leaching out through portals of exit, causing lesions of endodontic origin, apically and laterally. I'm very lucky, aren't I? [chuckles] What if that POE, that portal of exit, what if it was more around the lingual side of the route? What if it was kind of in an inaccessible place technically to get to, to cork it? So, I'm very fortunate it's right there and the palpation kind of gave me that sense that I might be able to see it.
So, we'll clear the board and that's what we can see. Here I am with my apicoectomies, so I've got the Lindeman bone cutter, got that right across those roots, got a nice flat table. You can see mapping the buccal root, nice flat table, mapping the lingual root. I've prepped down with a long, a surgical length ultrasonic tip. And I'm able to go up five millimeters and remove--follow the canal, track the canal. You don't really see a canal in here. I see outlines of PDLs. I see outlines of PDLs and I won't trace them all, but you really don't see canals. But when I got up here and beveled the roots with a diamond surgical tip, I can prep right up there. I could prep laterally right here and open that up and these two connect. This is down this way and then out through an L to this one.
So, we got two holes like that and I'm going to fill them out and get this thing corked. And if you slide it over, you can see we have the repair materials, apically corking and laterally corking. And if we do that, you can begin to see the possibilities. The possibilities are you can save a four-unit bridge. A four-unit bridge is worth thousands of dollars in Southern California. So, you're doing the patient a Hell of a service by salvaging a four-unit bridge. The aesthetics is not altered. We haven't further weakened the tooth, and you can see the bone has come in beautifully. Bone's not going to attach to the super EBA, but you can see maybe a little fibrous connective tissue. But look at how the bone has come in. Notice how we have an intact PDL in here again, and that's what endodontics can do.
So, properly performed, endodontics can be a cornerstone for restorative and reconstructive dentistry. This is a glimpse of what you'll see at the PCSP. So, I hope you got some value out of this and you begin to see the significance of endodontics and saving those bridges and splints and restored implants and saving those bridges and splints and restored implants. So that brings it to a close for me. So, I’ll see you next time on The Ruddle Show.