Over the past decades, many technologies have come to market to help dentists better perform each procedural step that comprises start-to-finish endodontics. Yet, many of these technological advancements...
TMJ, Lasers & 3-Rooted Maxillary Bicuspids Treatment Advancements & Diagnostic Considerations
Do you have satisfied patients? In this Opener, Ruddle and Lisette discuss what bothers patients the most and what you can do to help. Then, they go on to talk about a Specific Scenario: patients with TMJ and how laser therapy can improve comfort and mobility. Afterward, Ruddle is at the Board enlightening us on important diagnostic considerations when confronted with the 3-rooted maxillary bicuspid. Then, to close the show, Ruddle & Lisette decide to do something a little different and go on a field trip. Since Halloween is fast approaching, how about a visit to a haunted house?
Show Content & Timecodes
00:32 - INTRO: Top Patient Complaints 08:55 - SEGMENT 1: Specific Scenario – Treating TMJ with Lasers 25:24 - SEGMENT 2: 3-Rooted Maxillary Bicuspids 52:22 - CLOSE: Favorite Places – Franceschi ParkExtra content referenced within show:
- Palayam SG, Kurtzman GM: Laser Therapy for TMJ Problems to Improve Comfort and Mobility, Dentistry Today, 13 December 2024, https://www.dentistrytoday.com/laser-therapy-for-tmj-problems-to-improve-comfort-and-mobility/
- Ingle J, Taintor JF: Endodontics (3rd Edition), Philadelphia: Lea & Febiger Publishing, 1985
- Travell J: Myofascial Trigger Points: A Clinical View. In Advances in Pain Research and Therapy, Vol. 1, Bonica J, Albe-Fessard D, eds. New York: Raven Press, pp. 919-926, 1976
- RUDDLE+ Subscription Information: www.theruddleshow.com/ruddle-plus
- Franceschi Park – Santa Barbara: https://sbparksandrec.santabarbaraca.gov/parks/franceschi-park
‘Ruddle Show’ episodes & podcasts referenced within this episode:
- Find referenced shows within the You May Like tab above
Downloadable PDFs & Related Materials
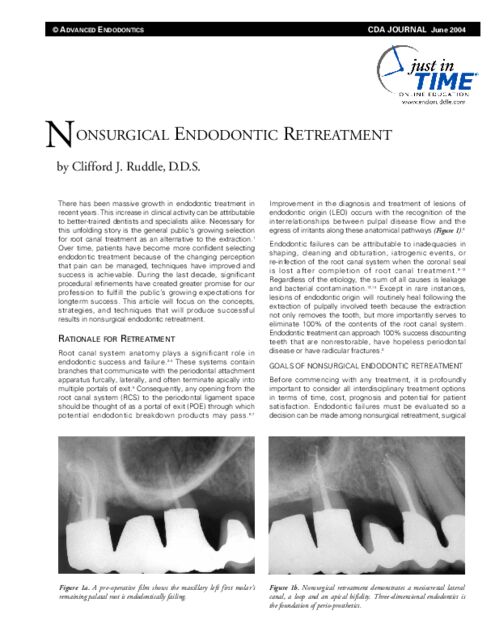
There has been massive growth in endodontic treatment in recent years. This increase in clinical activity can be attributable to better-trained dentists and specialists alike. Necessary for this unfolding story is the general public's growing selection for root canal treatment...
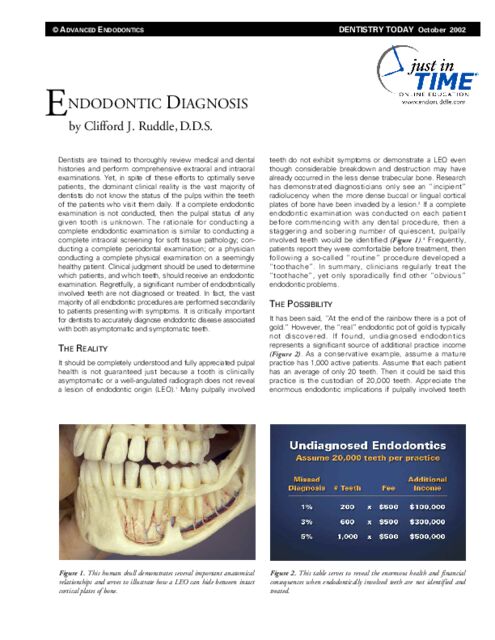
Dentists are trained to thoroughly review medical and dental histories and perform comprehensive extraoral and intraoral examinations. Yet, in spite of these efforts to optimally serve patients, the dominant clinical reality is...
Mao Tse Tung wrote, “The foundation of success is failure.” Clinicians who strive for endodontic excellence appreciate the elements that comprise success and use these criteria to evaluate the causes of failure. Endodontic failures occur for a variety of reasons...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
OPENER
…Before we get into this, why don’t you just give us a quick review on lasers, because I know not all lasers are equal.
Do you have an hour?...
INTRO: Top Patient Complaints
Welcome to The Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How are you doing today?
Pretty good, how about you?
I’m enjoying the humidity and the storm and the warm weather. I think I’m in Florida.
For me, I’m just trying to not let the Dodgers bring me down.
All right. I wanted to also say thank you for joining us again. It’s great to have you here and why don’t you get us going?
Okay. We’re going to talk about top patient complaints. Of course you want your patients to be pleased with the treatment they receive and their overall experience in your office, and this will go a long way to keeping your existing patients, attracting new ones through positive word of mouth, and also it will be good for office morale if you have satisfied patients.
Oh yeah.
So what are patients complaining about? Well it might not surprise you that the number one patient complaint is just too long wait times. And I don’t mean just waiting in the waiting room, right? What else is there?
Well first I’d like to clarify something. It’s a rhetorical question to the audience. Is it a waiting room, is it a reception room, is it a greeting room? Waiting has a bad connotation, and I hear people in real world dentistry and real offices: oh, have a seat in the waiting room. Waiting room, I actually did some reading on this. It makes people anxious. Waiting brings fear because of something that lies ahead that they’re not looking forward to maybe in their minds. And then it devalues them; they don’t feel important. So when we say waiting room – let’s say waiting room if it’s a waiting room, but it could be a reception room.
But also I recently have experienced this. I waited in the waiting room and then I’m taken back to an operatory and I’m waiting again. And I’ve learned that it’s a convenient way to get a little bit more time for the office. And after I waited in that room for 10-15 minutes, I went to a second operatory – I hadn’t even been anesthetized yet – and I’m now waiting in that room. So there’s waiting in the reception room, there’s waiting in the operatory, and then of course what about reschedules? A lot of times people, either the doctor’s side or the patient’s side, they have to reschedule for whatever reason.
And so we really need to have a receptionist that is attuned to what goes on in the back office, so front office/back office. She needs to be familiar with procedures and then she needs to come from an attitude of let’s make this happen. Because it’s really disconcerting if you’re rescheduling patients and maybe they’re hurting a little bit. Or maybe something like in my mouth broke a little bit and you’re waiting for that appointment. So when we reschedule, maybe we should ask basic questions like how are you doing with your mouth? Is everything good? If we were to reschedule you, would you be okay until that appointment arrives?
If your pain level is above 5 we’ll try harder to get you in quicker?
Something like that. But anyway, there’s lots of waiting is what you’re saying.
Yeah, and it’s not just rescheduling. Also say it’s just come up for time for your yearly exam or something, or six-month exam, and you go to make an appointment and they go oh yeah, the soonest we have is like three months out. And you’re like what, three months? Okay.
So I guess it’s good to have waiting lists because I know a lot of doctors’ offices also have problems with cancellations, so having a waiting list would be beneficial to both parties. And then like you said, be strategic about how you schedule, prioritizing more urgent appointments. And then maybe even grouping similar appointments together for maximum efficiency.
I like that.
But another top complaint is too much paperwork. And you recently also had this experience, right?
You know, I chipped this one right here Doctor. And they go yeah, here’s the Manhattan phone book; would you please fill that out before I look at your chipped tooth? So yeah, we have to do it for medical reasons, for legal reasons; we have to document, I get all that. But it does seem like there is an endless amount of paperwork that has become enormous in recent years. Maybe we could have them do it online at home, maybe they could have their wife help them. Phyllis went online and filled out my whole thing so I never had to see it, but I hate paperwork. And we also talked on other shows, we’ve talked about if they are going to fill it out in the office, have the receptionist or somebody that really is kind go out and say would you like me to help you. And you just sit there like you’re interviewing them and the receptionist or the hygienist or the assistant fills it all out.
I’ve actually had some offices give me an iPad to fill it out, and that actually did create a whole new confusion for certain people that aren’t used to that kind of technology.
I got an iPad recently, and there were calls I didn’t know how to make.
All right. Well another top complaint is the cost. A lot of clinicians will tell you that they need to increase their fees because their overhead is always going up. Maybe they have the latest and greatest technology and this costs money, and they need to pass these costs on to their patients that this is the price of getting quality treatment and very personalized service; it costs this much.
Yeah, you pointed out a good thing. You’ve got these really high fees, right? You’re competitive with Joe next door and you went across the street and looked at Mildred and you checked it all out. And I walk into your office and you take a film and I’m sitting there for 7 minutes like vmmmmm, I’m vibrating. In other words they don’t have digital, the walls are dingy, the office is kind of dark, everything is tired and old. So if you’re going to have high fees and you’re making a statement that this is who we are and we’re state of the art, maybe everything from the toilet in the bathroom to the reception area, the business technology, the dental technology, maybe it all sings. And one thing I’d like to say about this: have your staff talk about this. While you’re waiting for the doctor to show up, this is a perfect time to say God, we just got CBCT; we’re so excited! Now we can do 3-dimensional bla-bla-bla; we got a microscope, we got NiTi! Whatever you’ve got that you’re really excited about, talk about it.
Yeah. I think that – well I thought about making a list for this segment, but then I started thinking. It really, honestly, just comes down to time and money, really. I mean there’s too much wait time in the waiting room or reception room, in the various other rooms, just to make an appointment. Too much time filling out paperwork.
And then I think that there’s always probably going to be issues with costs because dentistry is pretty expensive. I mean a lot of people need to get financing to pay for their dentist appointments. So I think that probably just a lot of communication about the cost, about how much time is going to be required, maybe get people more prepared to what they can expect so that then they’re not complaining and angry about it. Because they already were communicated; it’s going to take this much time, you’re probably going to have to go to a periodontist too. After you do the root canal you’re going to have to go back to your general dentist for the crown. I mean all of this, if you communicate it all then they’re a little more prepared for it.
And then like you said, just make sure if you’re going to charge high fees that you have a great office, you have great technology and it seems very professional, and that you’re giving top quality care. So that’s just what I think.
Three things that didn’t make our list, but it’s on patient complaint lists. And I’ll just say in closing it’s poor communication. Another one happens to be unprofessional behavior; maybe there’s a little but of abruptness or what’s perceived as rudeness. And then finally, results. When people come back and they have a little handkerchief or a bag and they pull out something that you cemented a while back. Be committed to communication. Have your whole staff be professional. Stand in the shoes of the patient with compassion and you’ll get it.
And then if you’re really about quality and high fees, then get the results. Try to get the results.
Right. Okay, so we have a great show for you today, and we even have a surprise field trip at the end. So let’s get to it.
SEGMENT 1: Specific Scenario – Treating TMJ with Lasers
Okay, so today we wanted to discuss a specific scenario, and that’s patients with TMJ or temporomandibular joint disorder. Now specifically we’re going to talk about how lasers can be helpful in managing pain caused by TMJ. This segment is inspired by a Dentistry Today article from December 2024, and it’s called Laser Therapy for TJM Problems to Improve Comfort and Mobility, by Drs. Palayam and Kurtzman. We will have a link to this article in our show notes, because it’s kind of lengthy but it’s a very good article. This article interested us because in the past we’ve talked a lot about on The Ruddle Show and our podcasts, about how lasers can be helpful to do various things in dentistry and endodontics in particular. But the good news is that lasers can now help patients with TMJ.
Before we get into this, why don’t you just give us a quick review on lasers, because I know not all lasers are equal.
Do you have an hour? All right, so lasers are really in the forefront of a lot of dental care in recent years; not just days, years. There’s a lot of procedures now being done by a variety of dentists. It’s usually general dentists. Specialists use lasers but more selectively, general dentists are using them for hard and soft tissue both.
So the first thing you probably want to know about lasers is you need to know about the wavelengths. It’s procedure dependent. You tell me the procedure you’re doing and there’ll be a more optimal wavelength. So without going into the whole range of nanometers, like the diode lasers for soft tissue, the hard tissue lasers, and then we have some in between. There’s this article, Neodymium; Neodymium. So that’s – what do you call it? Stoked up or jazzed they call it with YAG, Yttrium aluminum garnet. So get the wavelength. And once you have the wavelength down, what are you working on, hard or soft tissues?
Then of course I’ll just read a few. For soft tissue lasers, you can begin to see how this might fit into some of your procedures. You can do apthos ulcers, herpetic lesions… it’s very good at about 800 nanometers of light. Dry sockets, you have bloodless incisions, you can do little gingivectomies around exuberant tissue in small children, so pediatric likes it. Some of the stuff can be done without anesthetic. I can go on and on -- dry sockets, nerve repair, implantitis – we’ve talked about that on previous shows and in the context of this show, of course these low-level laser therapy treatments can be used for the four muscles of mastication.
So that would be soft tissue, and if you throw it to hard tissue, you can recontour teeth and do preparations with oblation. You can strengthen enamel, and I learned that from you. I had to go off on a little journey to see about that, but carbonated hydroxyapatite is what your enamel is, and when you put a certain wavelength of light, you can make enamel more impervious to caries. So for children this is really good; lasers for enamel strengthening.
Tubules. I have pain in my tooth, can’t brush, pickles, sour, sweets. You can occlude the dentinal tubules. Remember, there’s about 60-120 thousand per square millimeter at the level of CEJ. So if you can occlude those tubules, there’s no back-and-forth fluid movement to stimulate the pulp. So that’s pretty cool. And of course again in the context of this article, you can do bone work, tendons deep; you can get much deeper with these hard tissue lasers.
What’s the advantages? You heal faster, there’s less pain, a lot of the procedures can be done without anesthesia. But just for you hardhats out there that love to know the why part: light triggers cells. And the cells we’re talking about are mitochondria. And mitochondria inside them have chromophores. And chromophores when they get light absorbed from the mitochondria, they get stimulated and they start producing like crazy ATP; that’s adenosine triphosphate. That’s a building block for all new tissue, for healing and for regeneration.
So you can tell that he’s very excited about lasers. Every time we do a segment that involves lasers I know that you do hours and hours of reading about lasers and different research. We’re going to talk about lasers a little more in a podcast, but I think you told me that you might even want to go get a laser even though you’re not practicing anymore, just because it’s so exciting.
I need a laser in every room. And I need different wavelengths. No, I’m not an expert on laser. I want to make sure I say that.
Oh no, but you’re very interested.
But I’ve been – actually when Phyllis and I were on tour many years ago in Germany, we went to Ohm and we saw the world’s first dental laser. So it started back about 20 years ago and they showed me different procedures they could do with the lasers at that time. So I’ve been fascinated ever since, and then of course I got really fascinated with endodontic disinfection lasers.
And just to be clear, what you would use for disinfection is not what you would be using for treating TMJ -- totally different.
Right. And that’s back to wavelength, tissue – hard or soft, duration of time, and the power, the power. It’s measured in milliwatts, but it’s pumped out and gated in jewels per second so you have to know all these things.
What about TMJ? What causes TMJ and what is your experience doing endodontics on a patient with TMJ?
Well the causes of TMJ are multifaceted. Trauma is one of them, poor occlusion, posterior bite collapse or teeth that are orthodontically misaligned so you’re chewing, grinding and bruxing. So those are some of the causes. And females, you have menstrual cycles, estrogen goes down. You get pregnant, estrogen goes (up). What else? Menopausal, estrogen goes down. So those are big causes in women. In fact I should probably mention, about a third of the population that comes in and sees you, a third of all patients will have some level of TMJ, and women will be two times more than men. So I mentioned menstrual cycles, menopause, pregnancies. Don’t laugh, because the estrogen levels are off and when you have low estrogen, bones start to get sore, tendons start to lock up and there’s more pain reported.
So how do you treat a patient that maybe can’t open their mouth very wide, or they can’t open their mouth for very long or something like that?
I think in our previous segment we were talking about communication, costs and stuff like that, waiting. But all that you said is communication. You need to talk to patients when they’re brand new. You need to ask them after you get the formalities out of the way and the niceties; how do you do when you have a dental visit? Can you open pretty well? And they’ll start talking; yeah, no problem, or yeah. What if they say I can’t open very wide? Well then you need to listen, ask the questions. Can you do longer visits, shorter visits? So what I would always do is it would start with the exam. And we would literally palpate the four muscles of mastication. And if you can pull off a trigger zone, I know they’re not going to do very well in the chair, even if they denied that.
So what did I do specifically? Let’s just say there is some concern or some problem, some level of problem. Pre-sedatives before the visit can help people relax. People can be put to sleep as part of that A/B on sedatives. Shorter visits oftentimes are demanded. A lot of times bite blocks can be used; pedo – not the adult block but the pedo-block, the pediatric block, very helpful to have people rest on versus straining to stay open.
And what else? Short visits, pedo blocks, sedatives. And then if you palpate muscles and it’s really a problem, if it’s an emergency, you’ve got to get the pain taken care of. But if it’s just a consultation, you might want to refer them. Talk to the general dentist, that’s where they came from, and find out if they do some sort of TMJ treatments. If it’s beyond the scope of the general practitioner, fortunately here in Santa Barbara we have four dental schools just south of us a couple hours say, and there are pain clinics and there are lasers in those pain clinics, and they can start to use some of the things we learned about in the article.
Yes. So I’m just wondering; if you thought you had a TMJ issue, you would probably go to your general dentist first and then maybe they could refer you to someone that has a laser if they don’t, or someone that they know who treats TMJ. The Palayam and Kurtzman article goes into quite a lot of detail about how to diagnose it and how to document the findings. They also talk about how both low level laser therapy (LLLT), and high-intensity laser therapy (HILT), how they can both be used to treat TMJ. So how do you know which one to use?
It comes back to your exam. If you’re examining and you’re palpating muscles and it seems more superficial, you’re going to be able to use a diode laser. And even within the 630-980, that range, there are even more precise settings in nanometers that you might want to use. But if it’s superficial – I’m going to answer it that way – it’s going to be more your LLLT. If it’s deeper, you’re talking about bone and tendons and you need to penetrate through quite a bit of tissue, it’s definitely going to be – in this article they feature the Nd:YAG laser, and that was 1064 nanometers of light. Because it can go deeper than our superficial ones.
Okay, and I guess I saw in the article that somehow maybe tinnitus is connected to patients with TMJ. That somehow there’s a connection there. Is that correct?
There seems to be.
It seems to be that the low-level laser therapy can help with that as well.
It does. It helps in some case reports. Remember, people are people and there’s a myriad of etiologies behind all this. We’re not getting into is it acute, is it chronic, when they open does the jaw drift off? I mean there’s all these things to start. I mean jaws are supposed to drop right down, but if they start to have deviations in opening, clicking and popping, you’ve got a problem with the patient.
But one thing beyond the tinnitus, everybody seems to say the tonality of the skin got a little better; they said they became more comfortable. And whether they got complete relief, there was less clicking and popping in excursions.
Okay, so if you do choose laser treatment to treat your TMJ, I understand from the article it generally takes 3-5 treatments spaced one week apart, and that the laser fiber tip is used in a non-contact manner and held 4-6 inches from the skin. Is that correct?
That’s what the article was showing, and they actually had beautiful photos. I’ve even seen colleagues use an indelible pencil that’s water soluble, and when they get the trigger zones, actually mark the places on the skin so you know where to hold the light. And like you said, you’ve got to stay off it. It might take 5,6,7 minutes they said per spot. And then like you said, I heard sometimes even two times a week, but several weeks. And of course you’re talking to your patients; are they getting a little bit better, are they holding their own, or are they actually not responding?
So that’s some things about that. I’d like to say even though the article featured two gentlemen that were older and they had co-morbidities.
Oh, the case reports?
They had a lot of co-morbidities, it doesn’t really matter; the heart disease, hypertension, all that. I mean it matters, but it isn’t part of this necessarily. But they saw that these patients responded quite beautifully. They had less pain, they could open, and like I said redundantly, they had less clicking and popping. So the patients were actually thrilled.
Yeah, and I think I even saw something that the symmetry of their face even got a little bit better.
They had these deviations. You know, one thing I’d like to say to the audience. When you look at the literature, a lot of times you’re looking at articles. You can probably find this, but I want to identify John Ingle’s textbook: Endodontics (3rd Edition). In that textbook he dedicates the book to two pioneers, two giants. Everybody that’s listening to this show has heard of Louis (affectionately “The Root”) Grossman; Louis Grossman. He was one of the founders/fathers of endodontics in North America.
But the other pioneer was Janet Travell. She’s a physician, MD, and she wrote a whole chapter in that book. She goes through all the muscles and how you palpate them and how you identify trigger zones. And she thinks a lot of TMJ is muscular. So you can have primary TMJ, secondary muscular, or you can have primary muscular, secondary TMJ. So she really goes into this, and I would offer good advice I think. Everybody should read the work of Janet Travell. She was the authority internationally on pain diagnosis and pain management for TMJ.
Okay. Well it does sound like it’s pretty promising what lasers can do for TMJ. I find it encouraging for myself even, because I have some jaw issues going on. I don’t mention it when I go to the dentist, and I think the article said that most patients do not mention it. They say – they kind of think that this is just how it is, that you live with it.
They accept it.
And when I had my root canals, I already know that my jaw doesn’t like to be open for a long time. I actually had a little bit of worry about it, never even mentioned it to the endodontist, but my thinking is I hope I can get through the appointment with my jaw how it is. And I did.
See, this is back to that communication thing again. If you ask patients – like if your endodontist said to you, how do you do when you have ordinary dental work done by your general dentist? And let me be specific; is there any problem opening? And zip. You would say well, now that you mention it – and then you would start a conversation. So that helps me know better how to treat you.
Yeah, I would say a little bit, but I’ll be fine. That’s what I would say.
I’ll suck it up.
Yeah, I know.
Can you use the adult block with the car jack?
Well it does sound like it’s an exciting future for lasers in dentistry, definitely.
Yeah. I found it in my reading; like you said, I got interested all over again. I think the future of lasers in dentistry is enormous. We’re focused right now on soft tissue procedures dominantly, and some guys and gals around the world are doing hard tissues. But lasers in the future are going to replace much of what we do with the hard tissue lasers, like the Er:YAG. We can remodel teeth and change them, preparations, less pain, heal faster. But I think that hard tissue lasers will replace the dental drill and all the burs and drills, and it will replace the scalpel. And we’ll be into a new age where AI and nanotechnology drives lasers.
All right. Well thank you for that information. We’re going to talk more about lasers on our next podcast too, so if you’re interested you might want to see that.
All right, well that’s it for this segment. Thanks.
SEGMENT 2: 3-Rooted Maxillary Bicuspids
Great to be with you again. Today will be another little lesson on anatomy. I’ve talked quite a bit on podcasts and on other shows about various teeth that hold anatomy. Maxillary molars: we’ve seen four is normal. Four on maxillary molars is normal, but oftentimes we’ve shown five and six-system teeth. Dens in dente, up in the anterior regions. On the lower arch – I won’t go through them all, but we’ve noticed that second canal, mandibular incisors; it’s there about half the time, it’s more to the lingual. Our molars can be C-shaped iterations, we have yet to talk about that; we have a whole presentation coming up on how to manage C-shaped molars. We’ve talked about and will show cases on Radix Entomolaris, Radix Paramolaris. And back to the upper arch, today the assignment is to look at another little anatomical variation, and that would be your maxillary through your bicuspids. They are sometimes tricky.
If we begin to look thoughtfully at our pre-operative film, and for those of you that have CBCT, you’re going to be able to pick these up quite readily. But for a lot of people, they’re thinking those maxillary first molars. They have two canals, dominantly two canals, second molars dominantly one ribbon-shaped system in cross-section. So when we get used to seeing things over and over again, that’s what we look for. So remember, you only know what you see and you only see what you know.
So if we were to look at some of these – we’ll just fly in six; we could fly in a lot more or less – but you can begin to see distinguishing characteristics on a radiograph. So I want to come back and take well-angulated radiographs. And I always said take three well-angulated, different horizontally angulated pre-operative films. Straight-on, break the contacts, look at the cull area. You can see the cull area in here, you can see our spaces, our cull area, break the contacts, okay. But that’s just one angle. I would also say you could move the cone up to 30° for the mesial. That’ll throw roots around a little bit and all of a sudden you’ll start to see some of the characteristic features that are exhibited by a maxillary, three-rooted bicuspid.
If you look here you can see a little indication that doesn’t look just normal. But a lot of us are in a hurry. I wouldn’t say reckless, but they have two canals, I’m looking for two canals. Do I see two canals? Of course there’ll be two canals. It’s up front, it’s not so far back. So let’s get the anesthesia, let’s get the rubber dam on, and you’re drilling into the tooth.
And if you look at the bottom row, you start to see the misunderstandings. You look at this tooth, and of course there’s a molar. We’re going to look at the bottom row at another session. Because I started thinking just before this presentation, I can show all six and jam it in and go like crazy and it would be a nice glimpse. I can go a little slower and I could be a better teacher. And I’m going to show today the trump row; that means Ruddle’s the first guy in and I’ll be the last guy out.
But in the bottom row you can see where the misunderstandings. You’re doing full mouth reconstruction. You’re going to tie up a couple bicuspids in a splint. They need to be endodontically treated soundly, because the whole foundation is based on the abutments.
So you can see a little post and kind of short, squig fill in there. You look over here, a lot of extensive dentistry, a little misunderstanding, maybe some paste, maybe a little cone in something. Those are all three-rooted. And over here we have to talk now about the molar, but then what about this bicuspid? You can see there’s a big lesion in here.
Lots to talk about. No treatment. No treatment in the DB, something in the MB, a perf through the floor of the tooth, that’s a cone going out through the floor of the tooth. These are things we’ll come back and we’ll talk when we have a little bit more time to do disassembly and talk about treatment planning. And then of course there just happens to be a three-rooted bicuspid. So let’s get started.
I have some extracted teeth. I used to collect these and if I saw something unusual in my hand because we collected teeth, I would put them in certain jars, mark the jars, and then my staff would go behind me and they would methodically farm the field. In other words, they would change the solutions weekly, we would put in a couple drops of sodium hypochlorite, and the teeth were very, very nice to look at and work on.
So here’s one of them, and this is a three-rooted, maxillary bicuspid. It's kind of a stout little tooth, but let’s look at some stuff. You can see our scalloped CEJ. But notice this distance from here to here. From the CEJ to the furcation is a long ways. Why am I pointing that out? Because usually canals diverge off the floor of the tooth. So the pulpal floor is where the canals, the orifices originate. So if you think of it like that, you might be thinking ahead of time I’m going to have to drill a long ways from here to here. It looks like to me that’s about 2/3 and this looks like about 1/3. So you’re going to have to have a really good drill path – not left, not right, not buccal, not lingual – but really have it planned out well. And if you have CBCT of course it’ll be easier. But you need to start thinking about how you’re going to get in here.
Let’s look at another view. Let’s take this tooth and rotate it 90°. Just to keep track we’ll call this the MB, because that’s what it is. And this would be our DB over here, and then you’ve got your palatal root right there.
So if we rotate this tooth you can begin to see. Here’s our MB, you can see the DB, and here’s the palatal. Looks quite different. Notice these curves. Remember, when you see things like doglegs, when you see this dogleg (this isn’t a golf lesson) the canals are more curved than the roots that hold them. So when you see doglegs and roots, anticipate considerably more curvature when you’re going in to do your glidepath management.
So that’s interesting. And why don’t we look at it a little bit from another view. This is just flipping it around, so we’ll call this the proximal but it’s the mesial view. This would be the proximal distal view. And again we’ve got the palatal root over here and we’ve got our MB here. See the breadth of it? You’re almost thinking it’s like a little molar. In fact, as I was looking at some of the old textbooks they called them ridiculous molars. So three-rooted maxillary bicuspids were called ridiculous molars. They are like little molars with compacted anatomy. So you almost could imagine there might even be two systems in here if you got in here and started playing around, but that’s how they look.
I’ll never forget this, I will tell this story. A prosthodontist – his name is not important but it was Francis Johnson – he referred a case in to me many, many years ago; it may have been three or four decades ago. It was a three-rooted maxillary bicuspid. He had a four-unit bridge hanging on it. He said Cliff, this one looks a little tricky; I want you to help me out on this. Could you help me out? I went to my jar, I pulled out some teeth that looked kind of like what I saw on the pre-operative radiograph. And in those days I was not wearing scrubs; I was wearing a white jacket that said Ruddle on it. And in my pocket, my doctor’s pocket, I kept a three-rooted maxillary bicuspid. And all during treatment as I was working along I kept [gestures]. Because I wanted to remind myself how thin the roots are, how tortuous the roots could be. And so the shapes have to be modified from what we might’ve used to do or normally do, just to accommodate minimally invasive dentistry, minimally invasive endodontics, how about that?
So here’s how they look, you’re seeing them. Kind of squatty teeth, sometimes they’re long, sometimes they’re a little more bulky; I’ll show you a couple of skinny ones in a bit. But this one’s got some curvature; it’s quite interesting. And if you begin to put pulps in it that helps you. So we drop some pulps in here, Hess type pulps, and you can begin to see the anatomy and how these things look. Now you can start planning; you can start planning your access cavity. But remember the floor is up here so everything is going to branch off deep. I’d say that’s way up, and so you’re going to have to have maybe fiberoptic light to help you with vision. Loops, microscopes, all these things are going to help you see. And then be on axis; plan it. Sometimes we always say measure twice, you can only cut once.
Now you can deroof, because sometimes you have two chambers. You have the chamber that is more where you would normally say, CEJ level. And there’s you palatal root and off you go. Off you go. But now you’re going to have to come up through here and take out a little triangle and get a little better access and get up here deep. I’ll show you this on the next case, but this chamber now in the buccal root is much deeper than the chamber on the palatal root. Two pulp chambers, that’s what Ruddle is saying. So there’s one pulp chamber, but then you can divide it into a more superior and a more inferior chamber and then deep you’ll get your branches.
And then in this view it’s interesting to see how some of these little anatomical variations how easily they’re able to be seen in some areas and how you can’t see them in other areas. Areas means films.
All right, so we go to a case. Forget the molar, forget the molar; it obviously was done in another era of time. Anytime you see silver points in the buccals and gutta-percha in the palatal, that was not so uncommon in the 50s and the 60s and the 70s; before we really dumped the silver points that Jasper introduced and we moved over as a profession to all gutta-percha.
But looking at this tooth you can see there’s a restoration. I noticed there’s a pulp cap right here. So probably you can imagine the pulp chamber is extending up in here somewhere, and if you do a pulp cap, the clinician is telling you, I was pretty close to the pulp. So it could be a direct pulp cap, it could be an indirect pulp cap. And we’ve talked about pulp caps and we like that regenerative procedure. In this case, there’s a lot of pain. The tooth is vital, but it is lingering and the sensation lingers for almost a minute, and the patient has some heat as well as the cold.
If you look carefully you’ll see the furcation right in here. If you look even more carefully you can begin to start to see – you start to see this little line here and you start to see a little line over here. Those are the proximal fluting on the roots; it’s quite prominent in a furcated tooth. But there’s the furcal floor. So if you start to think about the access, we’re drilling up about halfway before we get to a pulp chamber. In this instance, all the orifices came off the floor at the same place, on the same plane. And so it’s all originating right in here.
But again, if you look at those teeth, or if you had one in your pocket and you’re doing this tooth, you keep getting reminded: these are thin roots. These are corkscrew roots. These are dilacerated roots oftentimes. So you can begin to see we’ve got to cut back on our shaping a little bit, but we shape so we can exchange irrigant and we clean so we can fill. So remember, shaping facilitates cleaning and shaping facilitates packing. So you get a nice pack and that patient should be set up for life.
We can talk at another time, what’s the fee for these? Are you billing it as a bicuspid? Are you billing it as a molar? Why don’t you think about that? I think you should bill it as a molar. It’s more than two.
All right, let’s look at another one. Before we do, I want to bring you back to – you know, it’s nice to show you one bicuspid that’s three-rooted. So my multimedia guy, he said well we have some more in the library, why don’t we go get them? So here’s some other photographs. These are actually labeled for you.
So this is the view that you would typically see on your pre-operative radiograph. Again, three angles; please, three angles. Treatment plan for no surprises. You can start on one angle. I get it; one angle can show you the pathology. If you did your vital pulp testing, your pulpal sensibility testing, you could condemn the tooth based on the radiograph and your clinical test. On the other hand, when you flip that tooth around and look at it from the palatal – we never get that view – you can begin to see it’s a little shorter than the buccal roots. That’s usually not the case on molars. Also you can start getting a sense of how thin these roots are in their mesial/distal dimensions. Again, your MB is a little broader and you almost wonder if it could sometimes have two.
But to get the proximal view, and you can see lateral canals, you can see apical portals of exit up in here, so it’s quite interesting. And by looking at these teeth and holding these teeth or looking at an anatomy, almost all dentists almost immediately, invariably, lock on to be looking for the anomaly. You know, the percentage is about half a percent, 0.5, and the most I could find was 6%. So the incidence of a three-rooted maxillary bicuspid is somewhere between .5 and 1.6%. So that’s quite a range, but 6% isn’t very often. It’s not so often.
Let’s look at a case that looks similar to this, but will give you some ideas of the anatomy. I keep mentioning this, but it’s not just access and finding all the orifices and the work is done. Most dentists today are putting a lot of emphasis on conservative shapes, but shapes that can be cleaned nevertheless. And so you need to understand your shaping will influence your cleaning. I don’t know what your methodologies are for filling, but shaping will dictate how you clean, cleaning will be limited by your shaping, and all this has to come together in a modern trifecta somehow so that we’re doing all the tenets of success: cleaning, shaping and filling.
So we can drop that last pulp in. This is why a lot of times you don’t see lateral lesions because a lot of times the lesion forms adjacent to the portal of exit, and if it’s right over the root you might not see it. You might have to get a CBCT or get another angle to start seeing the breakdown of the bone laterally. Remember, the lesions form adjacent to the portals of exit.
The stakes are pretty high now, because this is the case that I told you about with the prosthodontist. He sent me in this case and said I really need it. So it was a strategic tooth in the most funereal sense, because a lot is at stake. In Santa Barbara, every unit is about $1500 and that was back then. It’s more today. So you can see a 4-unit bridge is going to cost quite a bit of money.
Now the anterior abutment is on a bicuspid. Is it just an ordinary bicuspid? That’s the question. So when you’re looking at the film thoughtfully, start to see if you can see things. I’m pretty close to the board, but I see a little line in here, so I’m thinking there’s probably something like this. And then if I get back a little bit I go oh, look at this! This goes up like this and it goes around like that. And I’m going oh, what’s this? This goes up like this and it goes around like that. So I’m starting to see, I’m starting to imagine, I have trained my mind to be able to see this before I ever treated it. And if you can see it, you can do it.
So the access needs to be planned thoughtfully. You might be thinking this is the drill path. Actually the drill path has to be accounted for. The crown has been lined up for gnathology, but the roots remain inclined distally. That means be careful on your access because we don’t want to loosen the bridge anterior abutment from the prosthesis. Careful access
I got the bridge off. I guess you remember in an earlier segment I said a laser can even be used, a hard tissue laser can even be used to delaminate bonding materials and remove bridges. I never did that, but it’s something that laser people tell me is possible. I’ve shown in many, many shows, multiple ways to remove crowns, onlays, bridges and splints. And in this case we used the metal lift. But once I got the bridge elevated and off – I just had the abutments to clean up and clean up the intaglio of the crown so I can re-cement – but it gives me a lot better shot in here.
And if you begin to see the level – that’s the floor, so you can see kind of shadowing. This is the height of the floor right here, that’s the height. Here’s your palatal root over here, that’s your orifice. So here’s the height of the floor, but when the floor – follow a little developmental line, and then it’s going to go like this and it’s going to go like this. And we’ve talked about it in other shows, the 14 ideas to find missed canals, abhorrent canals, calcified canals. So this is another chamber. This whole point over here is this is a chamber, this is your main chamber, and then this orifice comes right off the floor, but these are down several millimeters. So it looks just like that example we looked at.
I’m just throwing some files in here real quick to demonstrate I found the canal, to demonstrate there’s work to be done, and now we would want to get the files out of there and get our reagents in the pulp chamber, and then be negotiating these canals very carefully with a viscous chelator. Once they’re secured and they can be shaped conservatively, then they can be disinfected in preparation for filling the root canal systems.
So if we slide in the post-op, you can begin to see the pre and the post and things make sense to you. But again, the preps are a little small. Notice the recurvature of the distal buccal. DBs oftentimes exit out to the distal. A lot of times clinicians get blocked, they grind files in, they start their shape here, and they’ve got a big shelf here and this is blocked and then we get a LEO, a lesion of endodontic origin. So subsequently we want to see films over time that show bone fill, bone repair, and that’s an indication that we’ve eliminated the root canal system.
So that’s the anterior abutment. Don’t forget Ruddle’s trick. If you’re doing a really tough tooth – I know this is crazy – you might just have looked at that tooth. If you had one you might even go to a textbook, you might even Google, you might go online to Chat-GPT and say show me some aberrant molars, show me a Radix Paramolaris, I need to see a few, I’ve got a patient with one. So you can do a little homework.
I told you the story many years ago about when I was in China. The Chinese students were doing oral scanners, and using CBCT, and they were making C-shaped molars that they treated on their hand with a polymer tooth on the bench before they saw the patient. That’s preparation! So that helps encourage success, doesn’t it.
So that’s the second one, and the last one we’ll show you for today is kind of a little bit different than I’ve been talking about. You might say where’s the three roots? Geez Ruddle, I see this one right here, that one’s nice. That one probably goes with this one. And then I see this one over here and it goes over here, that must be that one. I think that’s a two-rooted, two-canal banger. I think that’s what it is. But sometimes you can get into these “fused roots” and find divisions. Those still count as three-canal maxillary – maybe not three-rooted, but three-canal; make the distinction.
So it’s again a bridge abutment. Dentistry is doing a lot to replace teeth, it’s pretty exotic. Implants that are holding restorations, bridges, splints, veneers. We can do a lot, but there’s pulps in these teeth and sometimes they have to be eliminated to be successful, and that means it’s an endodontic chore. And when we’re thinking of it endodontically, we’ve really got to be sure of the anatomy.
You can even see – this is quite a mesial angle, so this is just about a straight-on angle. But you can see in this photograph we’re shooting more from the anterior. You’re seeing the whole canine, so here’s our canine; here’s our canine right here. So we’re packed [inaudible] part of the lateral, see the canine. But see, this clinician was very good. They could see that little indentation on the buccal, that little invagination of tooth structure. And if you’re an endodontist or a well-trained general dentist, that’s a tipoff. Why would they be making a little invagination, and after the prep get the impression, and then build that back into the prosthesis? That’s somebody that really understands their anatomy. So when I start to see that, I’m really impressed. And now I have to be very careful because this is going to be basically one channel up in here, this is basically a pathway over in here, and then back to the palatal side there’ll be the palatal canal. That’s what I’m thinking. If I can erase; permission to erase.
So it was a tricky one. It was a tricky one. If you look at this pre-op – hindsight’s 20/20 – but it’s pretty fuzzy in here. In retrospect, it was resorption. In retrospect when I got into this canal it was very, very hyperemic. It was vascular, it was bleeding profusely, we were going through files, blood was coming out of the occlusal table, it was swept off by the suction. And we kept shaping, going up sizes, going up sizes, it was still bleeding. It took calcium hydroxide treatment, another visit. See a lot of you don’t like to do that, have another visit. I don’t care if you do one-visit endodontics. I don’t care if you do two-visit. I’ve done many multi-visit. It doesn’t matter, it’s packed when it’s right. So calcium hydroxide is very excellent to give us hemostasis. It can react with residual tissue and it helps in necrosis, necrotic tissue, flushes out teeth a lot more effectively than tenacious granulomas type tissue.
So you can see that’s kind of a big system there on the palatal. It had a portal of exit that’s enormous. I don’t know how big that is in diameter relative to the one I actually put a file in. So a huge, and I would say significant portal of exit.
Now one single buccal, one single buccal. It goes up to about mid-root and it splits, and it completely divides. And it’s in a fused root, because why? We can see in the obturation, through the cleaning and the obturation and moving thermal softened materials into the vacated spaces. We’ve got a big anastomosis, we’ve got more connections and communications. So those two systems through anastomosis are communicating. That means it’s really important to be doing good disinfection.
I’ve mentioned the SmartLite Pro EndoActivator over and over. It might be a poor man’s EndoActivator. It was shown at the last – two years ago at the AAE meeting in Los Angeles it was shown to be just as effective as GentleWave. So you can buy a $100,000 unit or you can do a $2500 unit, but whatever you’re doing – it could even be a laser. I’m pretty excited about lasers as you heard, so I would think you could even consider enhancing your disinfection.
So we’re talking about anatomy, but anatomy means treating the anatomy. Well part of the anatomy is the lateral canals, the bifidities, the deltas, the loops, the fins, and the anastomosing.
So I hope you liked that, and I’ll leave you today with the old, famous expression. This came maybe more from the surgeon’s perspective, but I would think when you’re drilling into teeth and you’re making that glidepath up into the chamber, I would think measure twice, because you can only maybe drill once.
Thank you!
CLOSE: Favorite Places – Franceschi Park
Okay, so here we are. We said we were going to be on a field trip and we’re at a place called Franceschi Park. You can see it’s known for its great views, right Dad?
Yeah, in fact if you Googled it, for you people overseas, you’ll want to come to Santa Barbara and come here because we’re known for fabulous city views. We’re kind of up here on the riviera, the city is down in the valley.
We’re actually 800 feet above sea level right here where we’re standing.
Wow, we should avoid all tsunamis then. And then the mesa is the other side, so Santa Barbara is in that little bowl, so we look at the city, very intimate. We see the harbor and all the masts, the boats, that’s cool. Look across the channel and the islands are out there about 20 miles away. So this would be a perfect excuse for you to come visit Ruddle, catch a dinner, and see Franceschi Park.
Yes. Now to just tell you a little bit, you see a house behind us. This house was built in 1893 by Francesco Franceschi. He’s an Italian immigrant and he was a horticulturist, and that means that he did a lot with gardening and garden management, and he imported over 900 species of plants. So this is actually, a lot of it’s overgrown now.
Do we need to get Castellucci over here with this cactus and stuff to do a refurberation? Arnaldo!
Okay, so Santa Barbara has a very Mediterranean-like climate; very similar probably to Italy in some parts of Italy. It’s actually quite humid and warm today. So a lot of the plants he brought here – he brought a lot of orchids. I can’t even remember all the names of the plants, the various trees to this climate.
Anyway, no one lives in this house, and if you look at it, it looks like it’s in disrepair, and it is. It was actually sold – in 1927 Alden Freedman bought it. He was just a philanthropist, but he only had it for a few years and then he donated it to the city. Well the city hasn’t really taken very good care of it. The park area is quite popular; it’s 40 acres. There’s this area here where the house is, there’s another area on the other side, if you go up a hill there’s a whole other area up there. So there’s a lot of little areas and paths of this place, so people like that.
Can the group out there imagine in the 1930s and 40s this big rotunda are where we’re at? You can see some plaques on the wall about no swords, one nation, all the nations are together, it’s quite good. Little children shall lead them.
So yeah, he gave it to the city and then the city was responsible for keeping up the maintenance of the plants and the park and the house. The city didn’t spend a single dime on anything. You can see a lot of destruction around here. The city then decided just recently they’re going to raze the home and tear it down. There was an outcry that could be heard around the world, and the city is now not tearing it down but they also don’t know what to do with it.
They said it’s seismically unsafe; that they can’t renovate it. Okay, there’s also – now this is not confirmed but there are some rumors that this house is haunted. And sometimes there are strange lights and sounds coming from it. This is one of the reasons we chose this spot is because this show will air closer to Halloween, so this is where I’ll be sneaking around on Halloween night.
Do we have to worry?
No. Actually there is an issue with kids coming up here and vandalizing it. There’s been a lot of vandalizing of the house and breaking windows and stuff. They do close it off at night, but it’s just a little chain. It’s just a little chain link string of chain that doesn’t really keep too many people out.
The good news is though, not only do a lot of kids still come, but we see a lot of older couples. Even geriatric people, because it’s almost spiritual to catch a sunset up here.
I’ve even had my daughter Eva tell me that she’s actually banned from coming here. Because she was with some friends once who -
Let’s not go into that too much.
I know. Isaac and I just look at her and go really? You’re banned from this place? Okay.
So one other thing I wanted to mention about this – oh, I forgot now. Oh yes, okay. So one of the reasons how I first learned of this park was when I was 15 years old and you were teaching me how to drive.
[Laughs]
I was learning how to drive a Karmann Ghia and it had a clutch, and there’s a very steep hill right in front of the park. And I just remember being on the hillside with you having me use the clutch and the gas and going a little bit up, a little bit down. A little bit up to learn how to use the clutch. So this is my first introduction to Franceschi Park was that.
Well I thought she might have to navigate the hills of San Francisco – which she ended up doing – but she needed to know how to do that clutch thing. It’s right here is where you learned it.
So this is very close, actually, by our house. It’s probably about not even maybe a mile from your house, and maybe half a mile from my house.
But we live on the Riviera.
Right. And when I was running a lot in the mornings, this is actually on my path. It’s not unusual to see lots of deer around here, even in the daytime. Mountain lions have also been spotted. You had that experience with a mountain lion.
Chased to the edge of my life. I guess not.
So anything else you want to add about it?
Well I’m glad we chose this because it’ll give our viewers a little glimpse of the charm and magic of Santa Barbara. So come visit Franceschi Park.
Okay, well that’s it. Hope you enjoyed this little field trip. Just to remind you that sometimes you need to get out of the office, get out in nature, do something a little different. So that’s what we’re doing right now.
Yeah, and the sky is uplifting, all those little cat paws, there’s a big hurricane to hit Mexico, we’re getting the tail end of it so it’s all good.
Okay, so that’s it. Hope you enjoyed this and we’ll see you next time on The Ruddle Show.