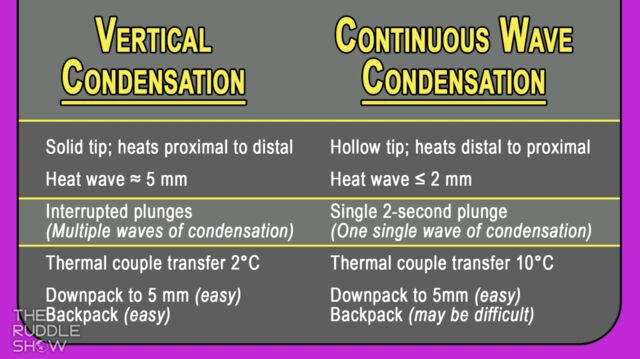
Featured Graphic from The Ruddle Show: Knowing the Difference - Warm Vertical Condensation vs Continous Wave Obturation Techniques
Insight & Problem Solving Comparing Obturation Techniques & Post Mishaps
The weather is warming up and baseball spring training is underway, but what does this mean for dentistry? Then, no season would be complete without a “Knowing the Difference” segment; obturation takes center stage when Continuous Wave is compared to Warm Vertical Condensation. After, Ruddle discusses post mishaps and how to manage them. Finally, the show closes with a Ruddle Rant; it has been awhile since Ruddle has had a chance to get some things off his chest, so be ready for some shock and awe ;)… and maybe a laugh, too!
Show Content & Timecodes
00:38 - INTRO: Baseball Spring Training & Dentistry Implications 08:07 - SEGMENT 1: Knowing the Difference – Continuous Wave vs Vertical Condensation 26:06 - SEGMENT 2: Post Mishaps 52:04 - CLOSE: Ruddle RantExtra content referenced within show:
- The Ruddle Show Graphic “Knowing the Difference – Vertical Condensation vs Continuous Wave” (see downloadable PDF below)
- Schilder H: Filling Root Canals in Three Dimensions, Dent Clin North Am pp. 723-744, November 1967
- AAE Discussion Open Forum: https://connection.aae.org/communities/community-home
‘Ruddle Show’ episodes & podcasts referenced within this episode:
- Find referenced shows within the You May Like tab above
Downloadable PDFs & Related Materials
Virtually all dentists are intrigued when endodontic post-treatment radiographs exhibit filled accessory canals. Filling root canal systems represents the culmination and successful fulfillment of a series of procedural steps that comprise start-to-finish endodontics...
There has been massive growth in endodontic treatment in recent years. This upward surge of clinical activity can be attributable to better trained dentists and specialists alike. Necessary for this unfolding story is the general public’s growing selection for root canal treatment as an alternative to the extraction...
There has been massive growth in endodontic treatment in recent years. This increase in clinical activity can be attributable to better-trained dentists and specialists alike. Necessary for this unfolding story is the general public's growing selection for root canal treatment...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
OPENER
…And then if we have them bite down and open suddenly it’ll pop the crown off. So be careful you don’t pop the teeth out.
Yeah, and I also said a minute, but I’m actually not sure about that number. So check the instructions…
INTRO: Baseball Spring Training & Dentistry Implications
Welcome to The Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How you doing today?
Pretty good, how about you?
Excellent, and I’m excited about the topic.
Right. So here we are going into the springtime again, and that means that it’s time for Major League Baseball spring training. Now I’m pretty excited for the new season, especially after the World Series last year. You might remember the thriller where the Dodgers beat the Yankees. So are you excited for the new season?
I’m very excited. I even dusted off my glove. It’s 60 years old, it’s a Rawlings and I can smell the grass on it. I can smell a little dirt and I can smell saddle soap, so it’s perfect.
Yeah, because we have a good team this year if you’re a Dodger fan. There’s quite a bit of interest around Hideki. I should say his name: Shohei Ohtani. Sorry, I said Hideki.
Not Hideki.
That’s another Japanese player. The Japanese are taking over the major leagues; I think they are. Shohei Ohtani is really a phenomenal player, and as those of you know who follow international baseball, he is a designated hitter because he had a problem with his pitching arm. He had surgery, what, a year and a half ago. So now he’s back on the mound, taking spring training, doing long toss and stuff. But it looks like this year he’ll not just DH; he’ll actually pitch as well.
I think he’s the only pitcher that both hits and pitches.
Except the Great One: Babe Ruth.
Oh, okay.
I mean there might have been others that we’re missing, but it’s more or less impossible. So maybe you have to go back almost 100 years to get back into the Babe Ruth era where they did that. But that was really cool.
Okay, we’re talking about upgrades and why I’m excited. They got this kid, this guy named Roki Suzuki.
Sasaki.
Sasaki? Oh, there’s another bad name. Suzuki in the Major Leagues. Sasaki. This kid is 23 years old and he was coveted by most of the Major League teams. But he ended up with the Dodgers, and that’s pretty exciting because we get to see him and Ohtani, and then there’s going to be one that you’re going to talk about. We’ve got Blake Snell; he’s a 2-time Cy Young Award winner. He’s joined the Dodgers this year and he’s back healthy. So things are looking good, because we had pitching health problems last year and it looks like we’re going to be a little better.
Yeah. I actually saw an interview last night. They were interviewing Roki Sasaki and he really wanted to come to the Dodgers because it was like his dream to pitch along Japanese greats like Shohei Ohtani; and then also Yoshinobu Yamamoto who is also an international Japanese pitching star.
Garvey -- he didn’t go to San Diego?
So yeah. I guess learning from your mentors, what could be more ideal?
So okay. We talked about how spring training works a few seasons back when we did a little opener on spring training. But maybe just remind – or inform our international viewers at least; what is the Cactus League and the Grapefruit League?
Okay, so if you know the United States at all out there – and many of you live in the United States – but this time of year, it can be snowing up north, it can be raining, it can be bitter cold. So baseball forever has gone south. They take 30 teams and more or less divide them by half. Half go to Florida; that’s where they grow citrus food so it’s called the Citrus League.
Oh, that’s the Grapefruit League.
Grapefruit League, yeah. They have a lot of citrus there, so they call it Grapefruit League. And then the other half goes to Arizona and that’s the desert, so they call it the Cactus League. So that’s pretty much where they play because it’s predictable weather.
Now what I’d like to encourage all of you to do – I’d like to encourage you to do it. I’ve had friends that have actually bought spring training passes that get you into any ballpark, say in Florida or in Arizona. And the reason you might want to go is you get to see everybody. You get to see the stars right up close, and there’s a lot of autographs and it’s just lower key, more relaxing. And the stadiums are throwback; they’re awesome.
The food -- I’ve heard the food is remarkable. So you might want to just go to the game to get the food, because the stadiums are beautiful, the field is beautiful. Everything’s beautiful and it’s a great way, pretty inexpensively, to see a lot of games in like a week or two.
You know, I actually saw a little bit of a spring training game last night on TV, the Dodgers. It was at Camelback Ranch and they said it was going to be in triple digits. So that’s very hot -- like 40° Celsius or something.
Wow!
Yeah, so it’s very warm there right now. Okay, so besides professional baseball starting, also Little League is starting. So if you’re a pediatric dentist, this might be your busy time. And I think we have another graphic; let’s bring that up.
Okay, so in our Season 10, Episode 6 I think it was, show, we had Dr. Beth Damas give a presentation, and she talked about some baseball dental trauma cases involving kids. Her son – she has a young son who plays Little League – and I remember she even spoke about treating one of her son’s teammates who I guess the baseball tipped off the top of his glove and hit him square in the mouth fracturing two of his teeth.
Yeah. The reason we liked that program, Lisette and I, is because it was really a call to action. Because if you know these kids, they’re like 8,9,10,11,12, they look like they’re all teeth. And especially the two central. I was going to say 8 and 9, but those numbers don’t work overseas. Anyway, the two maxillary central, they’re very prominent; they’re almost always going to get involved. So she gave us great ideas on doing pulp caps and pulpotomies so we could encourage root formation and maturation. It works well in mature roots that are young patients and immature roots, so that was really good. And people are still talking about it, so you might want to catch that show.
But also if we’re doing a call to action, we might want – if you have a kid and you’re a dentist and you have a son or a daughter playing baseball, maybe meet with the coach. And maybe meet with the parents and offer to do simple impressions and make bite plates or mouth guards so that you can prevent it, not treat it.
Yeah. You don’t even need to make impressions. When we had a mouth guard that was given to use at karate, you just actually boil it. It’s like a generic mouthpiece; you boil it for like a minute and then you bite down on it and it actually forms to your mouth. So you can have a specially fitting mouth guard.
I’m laughing, because there’s a – in a technical way of removing crowns there’s a little green “Jujubee” that we put in hot water. And then if we have them bite down and open suddenly it’ll pop the crown off. So be careful you don’t pop the teeth out.
Yeah, and I also said a minute, but I’m actually not sure about that number. So check the instructions.
Read the instructions; it never hurts.
All right. So all you pediatric dentists out there, be on alert; this might be a busy time for you.
All right, well we have a great show today so let’s get going on it.
SEGMENT 1: Knowing the Difference – Continuous Wave vs. Vertical Condensation
Okay, so it’s time for another segment of Knowing the Difference. This time we’re going to do it a little differently. Usually we do it at the broadcast desk, but for this particular topic, we thought it would be more powerful if you do it at this board so you can draw some pictures and that kind of thing.
So this segment is inspired by a quote by the 18th Century French author, Madame de Stael, who said, “Wit consists of knowing the resemblance of things that differ, and the difference of things that are alike.”
So with that idea in mind, today you’re going to compare and contrast continuous wave with warm vertical condensation. And believe it or not, there’s many clinicians out there that are not clear on the subtle, yet important distinction between these two obturation techniques.
So I will now step aside and you can take it away.
Thank you. I liked what Lisette just said, because knowing the difference, KTD; I would say most people just grab a heat transfer device, and they think it’s a piece of metal that is going to be used to bring heat from A to B. So most people just chuck up the electric heat pluggers – that’s what they’re called as we’ll see shortly – and they put them in different devices, heat transfer unit devices, and they have no idea how hot they’re getting, how they work. So let’s take a look. Let’s really zone in and think clinic as I’m describing a technical difference between two methods.
Well the one that’s been around forever is just called an electric heat plugger. And in this case, it is solid and that means that the heat would come in this direction and it would heat from proximal to distal. So it’s very important. As the tip begin to cool down, we have a heat sink. A heat sink is a greater mass of metal up in this region and it pulls the ions – the excited electrons – down towards the tip to keep the tip heated. That’s a critical distinction.
So our first comparison would be proximal to distal. Another comparison would be the heat wave. We have a heat wave, so if this is a piece of gutta-percha here – this is a root and now we’re going to go into a canal that’s tapered – the heat wave is about 5mm. So you’ll get a 5mm heat wave through your gutta-percha master cone, and it’ll come pretty much to the terminus of the cone. So you’ll get a 5mm heat wave. And I’d better write that down, huh? 3-5mm. And I’m going to erase that if I can remember how. It is a 5mm heat wave, so you have 5mm.
Some of you that have read Dental Clinics of North America and read Schilder’s article will see 5-7mm, and that has to do with we do interrupted heatings, removing gutta-percha, so the plugger can fit progressively ever deeper. And we carry multiple waves of condensation ever towards the terminus. So it’s interrupted, and that just means you have multiple chances to generate waves of condensation.
And as you do this repeatedly, that’s how you get the 5-7mm. Because if we were to look at a graph and this is temperature and this is time, body temperature is about 37° assuming you’re healthy, and we only have to heat gutta-percha up to about 40°. And at 40° it’s sufficiently thermal softened that we can put a plugger on it, and when we push when it’s been heated up, it is adaptable.
And then it begins to cool, and then we heat it again, and it begins to cool, and we heat it again; and you can see we’re kind of going up to this 40-45° heat sustained compaction cycle.
So that’s how we carry waves of warm gutta-percha deeper into the cone, push on the cone, adapt the cone, press on it while it’s cooling to offset shrinkage and then go in with a hot instrument, plunge in deeper, take out a bite. And please go back to the various Continuums. This has all been previously explained in our Shape•Clean•Pack Continuum. Also we’ve had various Ruddle Shows on the thermal mechanics and the thermal profile of warm gutta-percha with vertical condensation. So this is just a primer; it’s not supposed to be the deep dive.
Finally, if you put thermocouples out here on the root and measure trans dentinal temperature transfer, it’s about 2°. So I’ll just put thermocouple 2°C. That wasn’t considered dangerous whatsoever to the patient, because there’s a PDL. The periodontal ligament is moist, it wicks down the heat, so this is a very benign event if you’re talking about osteomyelitis or something bad happening.
Finally, when you have finished downpacking – when you have finished downpacking, the canal will empty. Except at the 5mm level, if this is 5mm. So we can try to make this a little bit more understandable. Okay, so you’ve got a root in here.
So that means if you need a post for prosthetic reasons, you already have a post space. It’s optimal; it’s a well-shaped canal. If in fact the case isn’t deemed to need a post, it’s very easy to backpack because the canal is empty. So you can go to the squirting devices and I won’t go into that; but you can squirt/pack, squirt/pack, and work your way out of the canal and backpack to the orifice, or just sub-orifice level so you can do part of that triple seal I’ve talked about on other shows; but that would be your orifice barrier.
So that’s a little bit about how that works. I guess we can get rid of most of this. All right, we’re getting rid of all those little dots of thermal softening, get rid of all this, and let’s bring in the next idea. Let’s now do the knowing the difference.
In continuous wave, which is obviously well understood and widely popular around the world; I don’t know if it was meant to replace vertical condensation, but it was deemed an easier and faster way.
Now we’re not hollow, so over here we must say that this is a hollow tube. So this is solid and this is hollow. By being hollow, there’s a copper wire that comes down through the device, the heat carrier, the electric heat carrier, and it heats this way. It heats distal to coronal. That’s just exactly backwards of what we just talked about where we heat proximal to distal. So this would be this comparison.
So that’s how that instrument is designed. The design was quite clever; it was to get around, I imagine, patents so that’s why the design is different. Solid is absolutely fine, but this is hollow.
Now what do we know about hollow? You’ll get a heat wave of probably less than or equal to 2mm. Because you don’t get much heat advancing because the tip is cooling away from the work where you need to tip to be softened to keep generating a wave of thermal softened gutta-percha. So in this technique, I said we had multiple, multiple times to get waves of condensation. Here you get one single shot. One single shot, and it’s a 2-second downpack.
So you start at the orifice level, sear off the cone, take a plugger, capture the maximum cushion of rubber. Sometimes canals are ovoid-shaped and you might be in an ovoid-shaped canal, so maybe you’ve got to throw some cones in around the master cone; or you fold the master cone over so you have a bulk of material to drive through. So you sear off the cone and then you go 1001, 1002, and you’re supposed to be down to the 5mm level. But the problem is if we get down to 5mm and we only get a 2mm heat wave, it means the apical extent of the gutta-percha master cone – if this is the apical one-third, we’ll just say this is 5mm, if this is your shaped canal – you’ll have a heat wave for 2mm. But this last 3mm is a single cone technique. It’s not thermal softened, it’s just its normal shape that came out of the box. So it’s kind of corking but not adapting.
So that means if you wanted to have a heat wave go to the end of the cone, you have to even downpack closer. And now we start to worry about overcoming our resistance form. Because remember, it’s the taper of a canal – it’s the taper of a canal that creates resistance form, so when we pack down, we get lateral components of force, and we get vertical components of force because the gutta-percha is grabbing these walls. As it grabs these walls, it prevents over-extensions.
So the problem is if you go closer, you could overcome your resistance form and you can carry your apical extent of your master cone beyond length. So that’s something that many people talk about and have been concerned about. Now I need to do a little bit of erasing. All right. This isn’t quite as efficient as the old 1950s eraser, but it works.
When they put thermocouples on the outside of the roots – this was on some of the earlier research – they showed that the thermocouple on the outside of the root measured 10°C. That’s quite different than 2°. And so there was quite a bit of alarm because we know that when bone meets about 10° elevation over body temperature, that means you’re going to get necrosis, osteomyelitis, and you’re going to lose the tooth probably, because the bone’s going to melt away from its support structures.
So that was then pawned off very nicely in some silicon papers that said basically, it doesn’t get that hot in the mouth. This was an invitro test, so there was no PDL around the root, nothing to wick down the heat. So the idea was maybe it’s not quite 10°; maybe it’s less. But the point is, when you go activate, 1001,1002; some colleagues go 1003 and they’re in there a little bit longer. So be aware of the rapid increase in heat on the external root surfaces when you’re doing continuous wave. Didn’t say it was bad,; didn’t say it was good; it just is. So you need to know that.
And the last thing; I think this is probably one of the most frustrating things I hear. You know, I had workshops in Santa Barbara for years, and we taught both techniques and I never told anybody what to do. They ran home and did whatever they wanted to do. But we had them do vertical on shaped canals, and we had them do continuous wave on shaped canals, and virtually everybody went home and did vertical because they trusted it.
You know, when you downpack…1001…1002… and now you’ve got a plugger sitting on top of a cooling mass of gutta-percha, you’re supposed to do a separation burst. So boom, less than a second, boom, activate, let go. And you’re supposed to withdraw the instrument and the body of gutta-percha is supposed to be circumferential around the electric heat carrier. So when you take out on the separation burst, your electric heat plugger, you’re supposed to see a big wad of gutta-percha. That means you have a post space or you could start to consider backpacking.
Well people know that do this technique all the time, when you do the separation burst as it’s called, rarely does all the body of gutta-percha get removed from the canal. Usually there’s remnants. Especially in canals that have cross-sections that are irregular. So you can plunge in here with your plugger, but when you go to remove this, oftentimes you’ll have some gutta-percha around it; but there’s gutta-percha left in the eccentricities off the rounder part of the canals.
Well that’s very frustrating, and that led to a lot of very convoluted techniques about trimming master cones and adding little sections piece by piece. Then all of a sudden, it became a product and you could buy these little pieces, custom made so you could backpack in through a tunnel with circumferential gutta-percha laying out here. And so many people preferred this technique, because when you take out a bite of gutta-percha, the plugger comes in – here’s you canal – and you step the plugger around the canal, scrape everything off the walls. And when you have a platform, you then press, and as you press, the walls are clean above you. The walls are totally clean above you, and what happens you’re downpacked; it’s clean. If you have a microscope you could look down and see a pink dot, and that’s like probably about 5mm away. And fortunately 5mm is probably sufficient in terms of how close do we want to get to length.
If you can get a heat wave through cone, 5mm. If you heat, remove, pack, heat, remove pack – two cycles. Heat, remove, pack – three cycles. By the time you do that, you’re getting closer to 7mm. Where do most curvatures live? Most curvatures you’re in the apical third. So you can pre-curve these to some extent; but remember, they’re metal. I didn’t mention this and I’m not going to go through all of this, but this has to be not just any kind of a metal. It’s an alloy, a very special conducting metal that gets hot almost immediately and can cool down almost immediately.
So a lot of technology in here. There’s different tip diameters, different tapers for both ones. So I’m just showing you an example, but I like to use the 40/05. The 40/05 is the only one I use in the Calamus System. So Calamus is what I’m using; before that, it was the Touch and Heat. B&L, they make heat transfer devices. So lots of companies make these, but know the difference. And the difference is the difference between getting more lateral canals. Because if you plunge in two seconds and you’ve got a great bit canal, you might not have enough mass of gutta-percha to hydraulically drive the sealer under 2000 PSI into the uninstrumentable, but cleaned out lateral anatomy.
So knowing the difference is important, and it’s the difference between getting more anatomy versus sometimes settling for less.
So here’s the cleaned-up list. I’ve been told I’m not always so neat and easy to understand with my writing. It got a little bit sloppy but it’s cleaned up and you’ll find the critical distinctions between continuous wave and vertical condensation in the show notes.
SEGMENT 2: Post Mishaps
All right. So we’ve all been doing dentistry for a lot of years, right? And patients come in to you, and you take films because they’re new patients and you want to better understand the path to oral health and what they’re bringing in that you might want to see. You’ve all seen the post that is mal-aligned.
So posts have three dimensions don’t they? They have length and diameter and direction. And sometimes – we can get this thing going – and this is a tooth we had fun making; it’s just for laughs. But it basically is to try to show many of the commonly encountered iatrogenic events, including posts.
So you can see the post is very large; it’s much bigger than the optimally shaped canal. I’ve talked about this for years. I don’t like those shoulders; there’s stresses that build up there and that predisposes to fracture. But a lot of times as these posts get placed in roots, we as dentists seem to forget external anatomy.
So we always talk about internal root canal system anatomy, but how many of us are talking about external anatomy? I’m talking about the root bulk and form and recognizing that a lot of these distal roots – if you look at these distal roots in cross-section, a lot of times they’re like kidney beans. And when you put a post in here, you’re way closer than you think you are. Because when you put a film packet in here and you shoot a film, this comes over and lines up there and these little things come over and line up there, and you’re thinking the post is well inside the root. But in fact it might be paper thin. So in this case, I’m actually showing a post perforated.
So today, to be very clear, this isn’t about how to remove posts. This isn’t about how to correct perforations. This will not be about how to do any of the post management things. We’re only going to look at post mishaps. And what we’re supposed to learn today, what I’m hoping you’ll learn today, is to measure twice because you can only cut once.
So let’s just look at some posts for fun. These are all done for laughs, and for my international group, yes I’m laughing very hard as I see these posts coming up. This is not an indictment on any particular clinician; it’s an indictment on the profession who trains clinicians to go out and learn to do things like that. And of course to be fair to the schools; no school is training dentists to do any of this. But see, you can begin to see how training deficits show up as mismanagements.
So that might be a silver point, to be honest with the audience; that’s probably not a post. Somebody was looking for the DB, so they got the MB, right; they got the MB canal, they got the palatal canal. Ahh, there’s the DB; and they trifidized off the occlusal surface of the third molar. Isn’t that great! Loved it!
You can see posts that go out the side of their root. In fact they recognized it was a perf; they took the post out before cementation and even beveled the post so it would be flat with the root and they sealed it. But the problem here with these ideas; they’re misdirected. There’s no endodontics. So why are we putting posts in teeth that had no endodontics?
Sometimes we think we can go deeper and bigger, and deeper and bigger is better. But a lot of times then we have frank lesions that develop, and posts, if you don’t have the ferrule effect, all the loads go right into the post and the post can split the root.
This person lost their crown. They came to the dentist, he said the crown’s loose. No problem; I’ll anchor it. So three massive screw posts, and the screw posts in the mesials aren’t even in the root. Broken instruments, and you can see that crack there.
So post mishaps. These might be kind of on the range of ridiculous, but we’ll look at some that are a little bit more subtle. Here we go; we’re going to look a three cases today.
Be sure to take your CBCTs if you have them. You get your 3-dimentional imaging, coronal slice, axial slice, proximal slice, or sagittal. You can take your conventional digital films, and maybe you have analog still, but digital is what we use. And I’m always saying three angles -- straight-on – we’re talking right side, straight-on, mesial up to 30°, distal up to 30° - and those three angles will give you more information than a single angle alone. So you can begin to see through your imaging what’s in the tooth that’s been previously treated.
So if you look at this tooth closer you can see there’s a bridge in here. I think it actually didn’t fit very well, so the idea was we’re going to section this bridge. We’re going to take off the leaky crown, because there was a leaky crown here. And necrosis, you can see the frank lesion apically; you can see that. The canal is observable, so that’s good news. So it’s not a hard case; it’s treatment planning. But what I want you to remember: this is Bridge #1. Bridge #1.
So I section the bridge just anterior to the distal abutment. I take off the leaky bridge, clean out the decay; the tooth’s broken off but it’s easy to get a ferrule effect, there’s plenty of super-gingival tooth structure. So basically it’s a simple kind of shot down there -- very easy kind of endodontic case. The request on the referral slip was please leave a post space. So I left a little cotton pellet in here, I temporized the top of the tooth; because the patient is literally going out of my office over to the next office to have the restorative effort. It was a pre-planned, dual procedure between two offices. So that’s what we wanted to do. And the patient knew all about it and so the work was done.
Probably six months later the patient called and said they needed to make an appointment with Dr. Ruddle because their tooth was sore, the one that Dr. Ruddle worked on. And we said did you go to the general dentist first to just make sure it wasn’t a hygiene or an occlusal problem or something? Yes, but the general dentist said there’s something wrong with Dr. Ruddle’s root canal.
Well there certainly is. Because this root is basically – on a long axis, it’s up and down, but the post is off axis. And this is just being in a hurry; this is just not taking the time. I mean this is a straight shot in here. I mean it doesn’t ever get easier than that. In fact, when you use burs, if you want to enlarge the canal prep – I say don’t; I say make your post fit the canal shape because the canal shape is already optimal. We want to maximize tooth structure; we want more dentin – as much as we can have. So the lateral dentin is really important.
So the shape’s not too big, it’s not too small; it’s root appropriate. It’s more conservative than we’ve talked about -- the rule of thirds, the rule of thirds, the rule of thirds. There’s way more tooth structure than a third/third/third. So we’re loving it all.
But now you see the breakdown is laterally a third of the crest. So the drainage is coming right out of here. So what are we going to do? I was pretty upset about it, so I thought maybe just tell them to have the tooth extracted.
So I started telling the patient that there’s a problem with your tooth. The doctor was right. Your symptoms are explainable looking at the film, and during the restorative treatment, there was a little mishap that I think we can correct. So I’m telling you; I’m communicating honestly. I’m not saying your doctor went out the side of your root; your doctor perforated your tooth; your doctor is now going to be in detention for several years as this goes through the State Board of Dental Examiners. No, you just say there was a little mishap with the restorative effort, but I think it’s fixable. And then when we talked about what that might cost and when we talked about what the alternatives might be, the patient was right back to I want to save my tooth. So that was the whole point.
So if you go to the Continuum in RUDDLE+, there is the non-surgical retreatment section. And we have a huge section, a very large section on lateral perforations and you can find out there. All the mechanical steps, the bleeding issues, the barriers, the backstops; that’s all discussed. So I’m just saying quickly today that we had to take the bridge off. It’s going to require another bridge – that’ll be the second bridge – and basically get the post out, wasn’t so hard. And although the post didn’t frankly go out the side of the root radiographically, there was an internal perf. And that’s because if you do a cross-section through here, the root is shaped kind of like that and here’s the canal.
So the concavity -- it’s probably perfed at the concavity. But again on the edge of the root you’re saying looks like it’s a little short -- probably still inside. Well you know it’s not still inside, because it broke down and there’s a lesion.
No fractures were detected; that was good to note and that was discussed. So as you disassemble, with the microscope you can see more and more. As you take out the bridge you can look and then you can take out the post and keep looking. Then you can look down at the bottom of the post hole and you can use acid etch techniques to clean that up. We used the gel that I talked about in surgery. It’s a preparatory for dentin; it preps dentin and removes all bacteria. It’s very, very nice; you’ve used those routinely in your bonding procedures.
So I’m just skipping to immediately post-op, so now we have – that bridge is basically in here again. I put the post in this time. Notice I chose a tapered post whose working diameter is really no bigger than the shaped canal. It’s just a blending flow from a metal tapered post to gutta-percha that’s tapered.
I used a little barrier in here. I didn’t need very much, but I worked all internally. I could push a barrier CollaCote. But I’ll again refer you back to the other Continuums where you can see me do this. We have photographs of me doing this, there are some videos of me doing this, there’s all kinds of documentation. Today we’re just saying that’s what we did. Post mishaps. So will it work?
Then we had the patient come back several years later and you can see the bone’s come in laterally quite tight. But we never lost attachment. I’m sure I could have probed really hard with anesthesia and probably demonstrated pocketing. But just going around, it was pretty much still intact, but you can see massive drainage. So this post mishap was handled by non-surgical retreatment.
This case is a case that’s been heavily restored, extensive dentistry, many, many hours of chair time. And you’re looking at all the crowns and the perio looks pretty good all in through here. I don’t know about right in here, but there’s a frank lesion here. I think the crest is sort of right in there; everything looks good. Apically I can’t really say there’s any frank pathology, but this is a problem. It’s a mesial lateral perforation, and that’s a large post.
So again we’re talking about anytime the canal is about this big and your post is this big – exaggerating to make a point – these shoulders are where you get fracture lines. So I would like you chairside just to bevel that and bevel that a little bit, so the post is no wider at its most distal end than the cross-sectional diameter of the shaped canal.
So what are you going to do? You could go in and do surgery, but as you think about this, you might be bouncing around on metal. And a metal bur on a metal post means the hole’s going to get bigger. We know that perfs on the lateral side of the root are enormous, because they’re elliptical. And we’ve talked in other bodies of work about A = πr2, so it’s not just a round hole we’re trying to fill. It’s round plus it’s now stretched, and it’s elongated, so there’s a lot of surface area that you’ve got to seal.
So what are you going to do? We started to disassemble. And what we’re doing is doing a lot of things here that are in other Continuums and other formats, but basically first you take the crown off, get the pin out, take the post out. I can use a lot of CollaCote up in here just to block so I don’t have any blood coming in, I don’t have saliva or oozing in here. I went ahead and I had a silver point to remove, and then I think the root’s somewhere up in there and somewhere up in here. The gutta-percha seems to be over on this side, so I see this distance and I see that distance. They’re unequal; remember the laws of symmetry?
So I have some gutta-percha to get out, but maybe there’s something else that would go over and explain the morphology that we see radiographically. I’ll try to draw it again. So the gutta-percha is not centered. Maybe there should be something like that.
So those are things that I’m thinking about. In spite of my efforts to turn the instrument around, put a little sharper curve on the file and try to explore something over to there, I could never demonstrate it. So we just shape that canal out and trust in our irrigations. Remember, dynamic irrigation moves irrigant into the uninstrumentable portions of the canal. You have an opportunity to have something forgiving that’ll help you be more than you were. So lots of irrigating, lots of activation with the EndoActivator, and boom.
I’m skipping many slides, but were able to downpack, bifidity. Got something over there; never got into it, but we got bifidity there. I could use CollaCote in here, I could pack CollaCote in here and have a barrier. And once I brought that CollaCote solidly so it would not compress upon intentional plugger action, then I can go ahead and use super EBA (ethoxy benzoic acid). That was the #1 here, that’s what was the repair. You today would have used biodentine, you could have used MTA, you could have used any number of bioceramic materials that are perfect in this environment. So that’s just what we did in that era, and again we were able to get healing.
You can see – it’s kind of dark in here, but now you can see the bone is right there. I see the bone here, I see the bone right there. You see a little tissue, a little tissue, a little tissue. But the point is the bone is great; it doesn’t probe. And if you lose this tooth, you’d either have to do a bridge or a single tooth implant, but the stakes would be a lot higher.
So what is expensive dentistry? Expensive dentistry is that dentistry that has to be repeated. It’s the dentistry that has to be redone again and again because it wasn’t right. So there’s never time to do it right, but there’s always time to do it over. Have you noticed that?
So we’ve looked at a second case, post mishaps. We’ve shown more of a concept on how to repair these and how to look at them, and we’re talking about exactly the nuts and bolts on how to do it. Those will be over at RUDDLE+ now.
But this will still get you excited. I think I showed this case to you some years ago on The Ruddle Show, but it was a dentist’s wife whose dentist did the endodontics and the post, so he’s with her. So now we have to have a conversation. He wants me to correct the problem is what he said. And I said are you aware of the scope of the problem, or would you like to talk about it? I know you’re a dentist. He said I’m retired, but yeah, let’s talk about it.
So I said well do you like the crown? Does she like the crown? Loved the crown; he did the crown. Is the esthetics good? Esthetics is fabulous. I said are you happy with the esthetics – to the patient. She said it’s very, very good. And it was good; it was very good. Smile line went up, didn’t see anything; everything looked good.
And I said so now you’ve got a post in there. The post probably would need to come out because there could be a lateral canal. There could be a lateral canal; it could be a fracture; it could be a perf. And he said well how would you know if it was perfed? I didn’t see any bleeding. I said let’s get another angle.
And remember I showed the picture earlier and I said take three angles: straight-on, mesial and distal. And again I’ll be redundant. You can move the cone not just a couple of degrees; move the cone 20° up to 30° so you can really get a different perspective. When you can start to throw the post closer and closer to the edge of the root, believe me it’s closer than you think.
And so if you look at a film coming in this way, just like that, that means that post is mesial. Well anybody in the audience could tell that it’s mesial, but there’s a big component that’s palatal. So it’s mesial/palatal, so what that means is when you’re talking to the dentist that did the work, you’re saying to them I don’t know if I can do surgery. Because he said can’t you go in there with surgery, clean out the granulation tissue, and if there is a post problem – which he said I don’t think there was, I never saw bleeding – then you can repair something. And you said you’ve got to tell him: if it’s on the palatal side of the root, I might not technically be able to approach it through the surgical site.
So all this was discussed, but we decided we would go in surgically because she loved the crown, we didn’t want to take the post out, the post has already weakened the tooth because it’s not going up along axis. Remember: length, diameter and direction. The direction is way off.
So surgery was indicated. Apically it doesn’t look too bad. But I want you to look at it apically again, because I read those things as early lesions. See a lot of times if you didn’t see this; if I covered up all this and all you did is looked at this x-ray, this single x-ray. You might say well, this one looks pretty good, this one looks pretty good. This one looked just a little ragged to my eye; but I also had more angles than I’m showing you.
So in essence, we laid a flap. And here we are making a combination attached gingival flap, full-thickness intersulcular flap. And as I pulled the flap back, there’s a huge break in the cortical plate. And you’re not surprised; that’s a huge chronic lesion. I have done a lot of granulation with the back end of the curette. Scoop it off the wall then go ahead and use the business side. Pull it out, here’s the hemostat; come in, pull it out; a massive wad of granulomas tissue.
Okay, so when I get that out, I can’t see anything wrong. The root has complete architecture. So I said to him – because he was with me during surgery – I can’t approach it. So I think we’re going to have to extract the tooth. And I’m going to make a proposal. If we extract the tooth and put it in the wastebasket, we could also consider extracting the tooth, and if I can do corrective work and address the problem, why don’t we replant it? He said that’s ridiculous! Nobody’s ever done that!
I said well there’s actually articles and chapters in books about intentional replantation. It’s been done before, it’s possible. I’ve done several; at that time I’d probably done about 40. So the more I talked, I said look. It’s not so much do you believe me or not, it’s going to be extracted. So what do you have to lose? If it’s going to be extracted anyway and you’re going to have to either tear this dentistry off and tear this dentistry off and do a new 3-unit bridge or do an implant. I don’t want an implant! My wife doesn’t want an implant. Okay, you don’t want an implant. So what are you going to do?
We finally extracted the tooth. This is the lingual. This is the lingual. Lingual. Now we’ve rotated the tooth around and this is facial. I want you to look very carefully at that root. Notice how black it is around the gutta-percha? It’s leaking; the whole root canal is leaking. It’s leaking coronal/apical and through the perf site.
Well where is the perf? You might say I see something maybe right in there. So we bring in another – you know, you don’t want to do a lot of curettage. That’s another lecture for another time, but you’ve already heard it in the Andreasen Tribute where we talked about replantation, trauma, traumatic injuries. But when teeth are avulsed you don’t get your curette out and start scraping the roots. You’ll completely have inflammatory resorption and the tooth will be lost. Andreasen says under water, lightly. Clean them just lightly, but with rinsing. No scraping. But we had to scrape off a little bit of tissue to even find the frank perforation.
So there’s the post. And now you can see why in the angle it looks like – in one angle, it looked like it was pretty much following the canal. Then I came from a much more mesial angle and I could tell it was mesial/palatal, and here is the palatal side.
So we have to prep this post back into the root and make a little preparation in here so we can cork it. I’m going to have to handle the end of the root; it’s leaking. This is all done extra-oral, so you don’t want a lot of extra-oral time to accumulate. And so here it is replanted.
So there you go. That’s how it comes in, this is your diagnostic angle that lets you know it could be palatal, and now you’ve done the intentional replant. But if you notice right in here and you notice right in here; there’s a little soft splinting. A little soft splinting. Because that tooth is conical; it doesn’t have a big root form, so we have to hold it in place. That would be the soft splint you can see in here, a little bit wrapping up in there, a little bit in there just to keep it stable. I don’t want it really solid; I want it to wiggle a little bit so the sharpies fibers can reattach from the PDL side to the root side that they’re accustomed to already attaching to.
And in closing, you’ll see that here we are. I think you would agree that if we went from this with a sinus track, post-op, it would look the same. Even darker probably, because I’ve scooped out granulation tissue. You can see we replanted it, so the PDL is a little bit wider over here because this is post work. But now if you come up the road about five years, the splint’s been removed, she’s happy, she’s esthetic, it’s healed in apically, laterally it’s come in beautifully, and that is pretty nice. And when you start to do that, you take frowns off of people’s faces and you replace them with smiles.
So in closing, I would like to just say to you; okay, so she has a nice esthetic; you can see that. I’ve got the lip pulled up, but when she smiles to her max, the most you see is about right in here. So she’s got a high lip line because she does show the whole incisal gingival dimensions of those teeth facially. So the gum looks good, everything looks good; all looks good.
So in closing, I want you to really look at those preoperative films and I want you to think, visualize – I used to say plan but if you visualize it, you’re planning – and then execute. So think, visualize, plan and execute, and that way, it’ll take you a lot closer to your full potential.
I hope you’ve enjoyed this section on post mishaps. Probably prevention would have been the better issue.
CLOSE: Ruddle Rant
All right. So it’s been a while since we’ve done a Ruddle Rant, so we’re going to close today’s show with the famous Ruddle Rant. Now what we’re going to do is I’m going to say a topic. Two of them are related to dentistry and then the third one will be a surprise, more of a personal topic, and you have one minute to say what you think about the topic. Obviously I’m not going to pick a very peaceful topic; I’m going to pick something that kind of gets your blood boiling a little bit. So are you ready?
I think I’m ready. I have a very nice, low blood pressure; everything’s fine.
Okay. Well these first two topics I’ll do, they’re both related to something you saw on the AAE Discussion Forum. So just to put that out there. So here’s the first topic. The first topic is someone posting something on the AAE Discussion Forum, maybe asking for advice or help from other clinicians, and they get no response at all. You have one minute.
I’m perplexed about dysfunctional forums. Okay, so a really respectable, reliable clinician posted a case, and she asked for opinions. The patient is asymptomatic; simply wanted to know should we retreat or not retreat, was referred in to her and they wanted her to retreat. So she’s throwing it back to you, this body of highly sophisticated people, well-trained, they walk with God in the clouds, and she asked for help. Days go by; nobody is answering. She says again, somebody give me an opinion. She probably didn’t even need an opinion, but she’s trying to get involvement, inclusive, gets you in there, gets you feeling good about yourself. But no, nothing more. And then another two or three days go by, still nothing. She prompts you again, finally one guy goes well, thank you for sharing. Didn’t really say what he would do or she would do. And then another one comes in.
You know this is – I didn’t say it, did I? I’ll just make my final point. Rick Schwartz, who is probably the most esteemed guy, quit the Forum because for a year and a half no respect, nobody answered. Okay, I’m done.
Okay. We can also go into this a little bit more on an opinion podcast.
What are forums for?
Okay, the next topic is someone was asked on the Forum why they did a certain technique that is not often done, and the clinician responded: because I have a lot of overhead.
Okay, so the bright one, the one that is always on the Forum, the one that carries the load on his lone back himself, posted a case about surgery and he used a bone graft. So that prompted a dear friend of ours, Arnaldo Castellucci from Italy, to write back: why did you feel it was necessary to use a bone graft? And he’s told a bunch of kind of funny little lines, but actually there was no evidence, there’s no scientific literature, we have no comparison studies. So he came back and finally said well, I have a big building. I have staff; I have supplies; I would close my office if I didn’t have a fee. Because basically Arnaldo was saying why are you doing a bone graft? For 45 years I’ve never used a bone graft! I’ve never used a bone graft for 45 years! Why do we need a bone graft? Oh my gosh. But he put a bone graft in a lesion and it looks like it’s healed on the post-op. Come on, you can’t even evaluate it properly. Where’s that minute? I’m going to get in trouble here.
So basically why are we – with the CBS thing on the implants, why are we when there’s so much distrust in the general public, why are we doing this?
Again, we can answer that question on our next podcast.
Let’s try to have some evidence if we’re using something.
Okay. Now here’s a more personal scenario here. So you’re on a walk and you see someone coming towards you up the street with a dog on a leash, and the dog is lunging and barking. And as you approach, the owner says don’t worry, he doesn’t bite.
Okay, so I live on the Riviera in Santa Barbara, and we have magnificent views of the city, the harbor, the islands. Oh my goodness.
We only have a minute.
The water – yeah, I only have a minute. And so you take these walks to get spiritual enlightenment, to free our minds, to think about complex problems and use critical thinking. And it’s not so good to walk by a fence and see a dog lunging and biting, barking, snapping at the metal fence.
So sure enough, I go around a corner and the dog that always does that to me, always barks at me, there he is and his owner’s got him on a leash. And the owner is behind the dog and the dog is coming down the hill, and the owner is saying don’t worry, don’t worry. He loves you, he never bites, he’s just friendly. And as we got closer I kept my distance, knowing that this dog did not look so friendly because I saw canines. And all of a sudden he leaps free of his owner and boom, he bit me in the elbow! It was a marvelous day. I loved how I felt the rest of the day; it brought great enlightenment to my day.
And that’s time.
Oh, okay.
Yes, that was a pretty bad bite you had; I remember seeing it.
Yeah. Those owners – you had a whole wonderful thing about dog-lovers and dog-owners. I forget how you worded it, but yeah.
Yes, dog people.
Can we do one on dog-sh*t or poop? That’s another problem I have on my beautiful morning walks is seeing owners let their dogs freely defecate across the road that I have to walk on.
Okay, we’ll save that one for the next Ruddle Rant when we return to the whole dog idea.
Okay, we’ll go to the dogs. Everything’s going to the dogs over here.
All right, well that’s our show for today. Hope you enjoyed it, and we will see you next time on The Ruddle Show.