Here are some ideas how you can improve your dental marketing by incorporating ChatGPT...
The Future is Now AI in Dental Marketing & Intentional Replants
If you are a dentist looking to escape the usual dentistry job, we have an idea for you; how about taking your talents to Federal Bureau of Prisons? Then, Ruddle and Lisette return to the AI discussion, this time talking about how you can use ChatGPT to maximize your dental marketing. After, Ruddle is at the Board, fascinating us with a seemingly futuristic procedure: the intentional replant. Then, it’s time to hear what Phyllis is thinking about regarding facing challenges and being the better for it.
Show Content & Timecodes
00:34 - INTRO: Prison Dentist 07:11 - SEGMENT 1: AI – Utilizing ChatGPT to Maximize Dental Marketing 19:17 - SEGMENT 2: Intentional Replants 47:23 - CLOSE: What Does Phyllis Think? – Facing ChallengesExtra content referenced within show:
- Special Guest: Phyllis Ruddle
- Federal Bureau of Prisons: www.bop.gov
- “Face/Off” – Action Thriller Movie, 1997
- Ruddle Show Graphic “ChatGPT Dental Marketing Ideas” (see downloadable PDF below)
- Ruddle Show Graphic “ChatGPT Pros/Cons” (see downloadable PDF below)
- Winans X: How AI is Changing the Game in Dental Marketing (and How You Can Use It Too), Dentistry Today, 27 November 2024, https://www.dentistrytoday.com/how-ai-is-changing-the-game-in-dental-marketing-and-how-you-can-use-it-too/
- Duke Women’s Basketball (YouTube Channel): “Kara Lawson: Handle Hard Better,” 5 July 2022, https://www.youtube.com/watch?v=oDzfZOfNki4
- Strayed C: Wild: From Lost to Found on the Pacific Crest Trail. Alfred A. Knopf, 2012
‘Ruddle Show’ episodes & podcasts referenced within this episode:
- Find referenced shows within the You May Like tab above
Downloadable PDFs & Related Materials
Here are some of the pros and cons regarding utilizing ChatGPT...
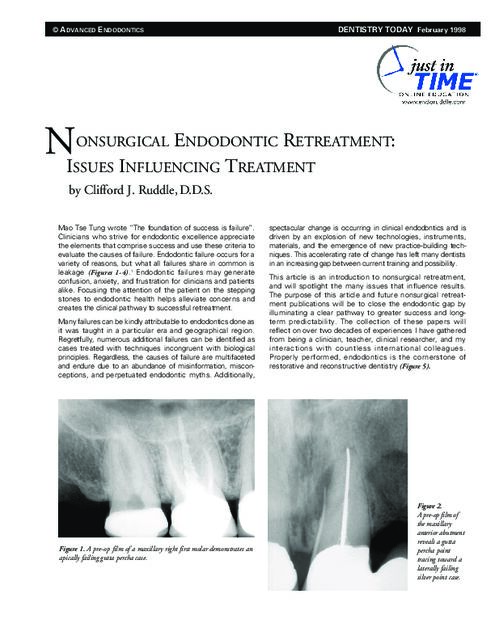
Mao Tse Tung wrote “The foundation of success is failure”. Clinicians who strive for endodontic excellence appreciate the elements that comprise success and use these criteria to evaluate the causes of failure. Endodontic failure occurs for a variety of reasons, but what all failures share in common is leakage...
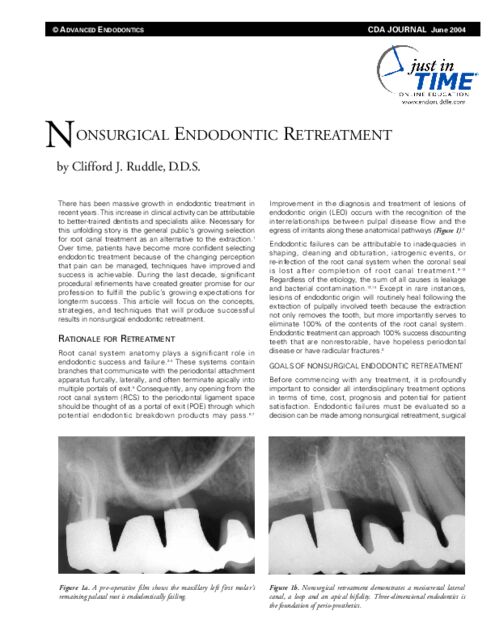
There has been massive growth in endodontic treatment in recent years. This increase in clinical activity can be attributable to better-trained dentists and specialists alike. Necessary for this unfolding story is the general public's growing selection for root canal treatment...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
OPENER
…So you can then use this information to fine tune your website. And how would you do this?
Me personally?...
INTRO: Prison Dentist
Welcome to The Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How you doing today?
I’d doing pretty good, what about you?
Excellent, and I hope the audience is absolutely thrilled to join the show. Right?
Right. Well today we wanted to go back to a job idea. So maybe some of you are tired of your normal routine of practicing dentistry day after day in your quiet office. Over the years we here at The Ruddle Show have tried to give you some ideas about how you can use your dentistry sills in more unconventional ways. We’ve talked about the possibility of becoming a hockey team dentist, getting involved in forensic dentistry, and we’ve even mentioned taking your dentistry skills to remote regions of the world to help out those who are less fortunate.
Yeah.
Well today we have another idea. This could be you. How about being a prison dentist employed by the Federal Bureau of Prisons? Who might be a good candidate for this kind of job?
Well if I was the warden and I was doing a profile, I would want somebody that is really interested in working in a vulnerable population. It’s got to be a person that because of their personality and their makeup they want to make a difference for others. So I think you need those two things. And then I think you have to really want to go into a more regimented environment. It’s not like throw your knapsack over your back and go into your office every day. There’s going to be some security and different things, and long walks and finally arriving. So you have to be willing to do all this kind of stuff.
And you’ve got to be able to relate to criminals. I hate to say it, because maybe you’re not a criminal. Maybe you used to be a criminal. But it helps to understand that they have very diverse backgrounds. If you think of the prison population – and there’s a lot of them in prison – they come from all walks of life. So you have to be able communicate well, you have to be able to be vulnerable and put yourself into awkward situations. And I think probably most of all you need to be able to really want to help turn lives around. This sounds corny, but my dad was a minister and he did a lot more than ministering. I saw how he helped people with gutters and roofs and all kinds of stuff. So in prison you’re there to do dentistry, but there’s many things you could say. Maybe they start making a record of what they’re doing, maybe they start reading and maybe bring them a book, and maybe bla-bla-bla. But you have a chance to change their lives around.
Okay. Well according to the Federal Bureau of Prisons website, it’s a very safe and supportive environment with opportunity for growth. It has a very competitive Federal Government salary with benefits like retirement and healthcare. And then there’s also opportunities for loan repayment and the flexible work options. So how do you go about getting a job like this?
Well when you work for the Federal Government it’s pretty much pre-ordained, right? You are going to start with filling out a lot of paperwork and they’re going to want to do background checks because you’re in security when you are there, if you’re working there. So you’ll fill out a normal government application. They’ll tell you all the prison sites in the country and then they’ll tell you the ones that need prison dentists at this moment. You have two choices; you can put down your first two geographical regions at that point, or you might want to move, who knows?
But anyway, that’s kind of how it works. They matriculate your application, they do something behind the scenes – probably a background check and qualifications – and then finally if there’s an opening, they notify you.
Yeah, I wonder if there’s a lot of turnover. Anyway, when we were discussing the segment there was a lot of things we were curious about. We were wondering what techniques they do, what technology they use, and then this actually motivated you to go do a little research on your own. So what are some of the things you found out?
Well after I watched the movie Face Off – no, just kidding. Actually they do simple things. Prison dentistry isn’t about full mouth reconstruction; it’s about taking care of what’s going on right now. So they’ll do things like simple extractions, they’ll do fillings and restoratives to some extent, they’ll do cleanings, they’ll do scaling and root planning. And if you’re a prosthodontist who got tired of practice but you love doing removables – removable dentures or partial dentures – they do a lot of removable and partial dentures. What they do not do is they do not do implants, they do not do crowns, laminates, bridge work. They do do some simple root canals. Because I found out what they don’t do is when the root canal is failing it gets extracted. And what they do refer out are difficult impactions, third molars. If they themselves are taking a tooth out and they break something, that can get referred out of prison. And what was the other one? That was it; impacted molars, failing root canals and root tips, stuff like that. They’ll refer that.
Yeah, I’m wondering if they do preventative checkups. Like every year you have a dentist appointment and a teeth cleaning or something like that.
I don’t know.
Well one thing that I think is the most interesting, and that is if you become a prison dentist at a maximum-security prison with the worst of the worst offenders, one thing probably for sure is you’re going to have a lot of interesting stories to tell I’m thinking.
Yeah. I had a classmate – his name is anonymous – but many years later after we graduated, decades later he got into some trouble and actually Phyllis and I went to Lompoc Federal Prison to visit him. And while we were there he actually said to us – I was thinking about this the other day – he actually said it might be good for me to come back and donate maybe a day a week or something to be a prison dentist. Because he said I met a lot of people in here and there’s a lot of interesting people and they need help. And he kind of became spiritual; the thought through that little avenue you might shine some light, bring them a Bible to read or something like that.
Okay, so there’s another idea for you. We have a great show for you today so let’s get to it.
SEGMENT 1: AI – Utilizing Chat GPT to Maximize Dental Marketing
Okay, so today we’re back to artificial intelligence. Now AI has become such a dominant force in our society in the past couple of years that I don’t think we really need to explain to our viewers anymore what it is. Probably most of you have heard of chatbots, like Chat GPT is the most common. But there’s also others like Claude, Grok, Gemini, to just name a few. Today we’re going to say Chat GPT, but you can substitute your own chatbot if you want. Over the years – I guess it’s been years now that we’ve been doing The Ruddle Show – but we’ve talked about how specific AI software can be used to diagnose caries, fractures, oral cancer. We’ve talked about how AI can be used to predict tooth loss and peri-implantitis. We’ve talked about how you can incorporate AI into your practice, and we’ve also even compared some AI systems.
So today we’re going to talk about how you can use a chatbot like Chat GPT to help you with your dental marketing. Have you ever used Chat GPT yourself?
Well I liked the word “GPT.” I didn’t know what it meant exactly and it’s used all the time. But I liked the words “generative pre-trained transformer.” Generative sounds like it’s going all the time; it’s like regenerating, making the future. And then pre-trained sounds like there’s somebody that’s going to help you and they’re trained. And then I liked the transformer because you’re transitioning; you’re evolving as you work with it, so I liked that.
Actually no, to answer your question. But just so you hear me; I’m very interested in it going forward. Over the last two or three years and having different shows, as she mentioned, it’s made me realize it could be very helpful in things I’m actually doing that we’ll talk about later.
So my version of using it is dumbed down. I would just use a Google feature and AI would come up and it would tell me -
An AI overview it seems like?
Yeah. It then says more, and you hit more and it can go to references, literature and other places. So I find it very efficient to learn quite a bit about something that maybe I’m not aware of, and then to get me to more sources. So that’s my vision; it’s a dumbed down vision of Chat GPT. It’s not generative and it’s not transforming me.
But my grandkids, Isaac – I call him affectionately the shooter – he has a machine and he has 3-D printing, he likes to do that. Well he is using Chat GPT, I understand, quite regularly, because it helps him with coding and then it helps him with his efficiency. So I thought that was very interesting. It gives him – we’ve had offline discussions, me and him and you, and I can see how it’s really motoring him forward. So that would be an example from one grandkid.
Another - your daughter, my other granddaughter, she works in cosmetology in a salon. And sometimes a product will be discontinued or they’re out of it, and she can go and with Chat GPT they can compare and contrast different similar products, fees, time, chemistry – because she has to know the chemistry because what’s it going to do when it hits the hair. So that’s an example where two grandkids are using it all the time.
Dangers? I have a list here. I don’t need to explain any of these other than to say the pros would be it increases efficiency, predictability, accuracy, quality. It decreases costs, that’s the whole point. The cons: some people are worried already here in the marketplace. I might lose my job. There’s ethics concerns: you can perpetuate this information and bias. Privacy issues: you have to be very aware when you’re working with your patients and you want to get some – you’ve got to protect the privacy, anonymity.
It has low emotional intelligence, so it’s going to take training to make it start to think like you. But that means you have to feed in to get it to think like you, because it’s learning about you. And then it can be misused as we said.
So those are kind of the pros and cons.
Okay, well thank you for that. Now we’re going to -
Isn’t she bubbling over today? My God, we’re doing a great show here on artificial intelligence!
Okay, so we’re going to get back now to how you can use Chat GPT to help you with your dental marketing. This was inspired by – this segment is inspired by an article, a Dentistry Today news article by Xaña Winans, and it’s called How AI Is Changing The Game In Dental Marketing And How You Can Use It Too. This article just reveals some very practical ways that you can use Chat GPT to help you with your dental marketing, and we’ll have it in our show notes. But you can use it to learn who your typical patient is.
So the author suggests that you upload a patient database into Chap GPT, minus the names and sensitive info. And then it can use that data, like the data of age, their spending habits, their income, and come up with maybe who your typical patients are.
So for example, your patient profile could be a working mother that’s looking for flexible hours; or a retired couple that’s looking for affordability. So you can then use this information to fine tune your website. And how would you do this?
Me personally? Well I would want to upload, if that’s the right word, my URL – that’s my address where my website is – and I’d want to upload that to Chat GPT. And I might want to actually ask a question: are we communicating with our patients? Not only our existing patients, but potential patients. So I’d want to know that.
And then I might also want to ask Chat GPT by asking specific questions and having the staff involved. What can we do necessarily that could affect more visibility and get better results from the general public? So as an example, if you like to do implants, crowns, bridge, that kind of stuff, you might understand there’s a financial implication with all those cool laminates and all that. So how do you get that message out that you do it, but yet it can be financed or it can be affordable? We’ve had shows where we’ve talked about how you can finance at the office as an example.
Maybe people have a hard time getting in to see you because they’re working their butts off. So you might have to say a little comment that I work one day a week in the evening, or I start extra early in the morning to accommodate schedules. And I might even take a half a day on the weekend, or a day on the weekend and transpose that day and take another day off. But availability would come to mind. And finally if you really love lasers and imaging, like CBCT, digital, it goes on and on, air purifiers, technology; you might want to tell the world about your technology and why your office is special.
Yeah, so that’s great that you can -
How am I doing?
No, great. So you’re trying to fine tune your website to be more to who your actual patients are.
That’s right.
Okay, well then if you know who your patients are, then you can ask Chat GPT to create a digital ad for you and then you can get feedback and see new options. You can even use AI to create a 30-day social media calendar, and the author suggests that you come up with a mix of educational content, maybe patient testimonials, what you’re doing in the community, community outreach, maybe some tips or recommendations, maybe even something about your office culture. So you can really do a whole variety of posts on social media and AI can help you do that.
So what do you have to be careful about though?
Well I think with anything we need to make sure Chat GPT – you know it’s generative, it’s helping us transform. We need to give it feedback. So it’s important that somebody on the staff or the doctor himself, but there’s usually somebody that’s good at this; they need to look at that and see how it’s projecting the website presence and then be working with Chat GPT behind the scenes to refine it so it begins to learn. Because it can do machine learning and it can learn more about what your responses are, so that’s helpful. And then patient anonymity has to be totally protected.
Right. Yeah, it does seem to me that – oh, I just lost my thought. But anyway, all of this is very exciting and promising. And I was asking my son, Isaac, about it because he uses Chap GPT a lot, and I said so do you pay for it or is it free? And he said that there is a free version, and then there’s also a paid version where you can create your own GPT. Because Chat GPT is very general, but you can create your own.
So I was thinking well wow! What if someone wants to ask Cliff Ruddle questions all the time? Well you can download all the articles from our website, upload them into your personal GPT, download all the Ruddle Show transcripts and paste them into your GPT, and then you can just ask what would Cliff Ruddle say about this and I’d be curious to see what the responses are like.
Yeah, imagine the time I would log on at the beach. Because now that I’d be freed from this vast vestige of responsibility of asking questions from international colleagues. I could just be at the beach.
But oops! I can see that that’s my new assignment and it comes with some responsibilities, so I would have to work with what you just said. And over a little bit of time you’d buff it out and polish it, and all of a sudden it would be pretty much what we said.
But I liked today that we’ve given you some glimpse of how you could use AI as an example, and Chat GPT in your practice to attract more patients. I liked the social media calendar and how you mentioned hashtags, testimonials, video clips and stuff like that, because that’s always really fun for other patients to see because they get ideas and it sparks action.
Back to one of your most exciting things that you told me about is if I could take all the articles you and I and your sister, that we wrote, and it goes even before you two daughters; if I could take all the articles we ever wrote and put them in. All the editorials, put them in Chat GPT. All the videos. If I could take all the questions and answers that came in. And if I would start working with that and start refining it, it could be pretty formidable for the future of education.
Yeah, it would be. And if you want to know more about this you should check out the article that kind of inspired us, because the author in that article gives you exact verbiage as a suggestion that you might want to ask Chat GPT. She really kind of in the article tells you how to go about it. We just kind of give you a general overview here, so you might want to check that out.
There was a quote I came across by Ginni Rometty, who is the former CEO of IBM, and I really liked this quote because it says “AI will not replace humans, but those who use AI will replace those who don’t.”
Ooh! So action -- call to action!
Okay, well I guess we gave some useful information, hopefully, and we hope you enjoyed this segment.
SEGMENT 2: Intentional Replants
Okay, all of us that are out there practicing. We encounter occasionally patients that come in with a tooth that’s been initially treated endodontically and it’s failing. So I normally used to say – and most of us do say as teachers – well you could consider retreatment. Well you could consider retreatment, and even if you needed to, you could advance towards a surgical approach. So that was initial treatment: strike one. Strike two was the retreatment, and surgery was three.
But then if that fails and the tooth is still symptomatic, we normally just extract the tooth, don’t we? So what I want you to consider is what if you could extract the tooth and do the corrective work in your hand and replant the tooth?
Now some of you might think this is crazy. What Ruddle is talking about? But there are probably in the literature 6,000 references – 6,000 – to the intentional replantation. There’s probably 600 articles roughly out of that 6,000 that actually talk about it. And there’s very few if you start to look at good papers and good methodology, there’s only a handful of papers that actually describe what I would consider something you could really consider.
So I’d like to just bring this back to the illumination of the international market, because if you’re going to throw it in the wastebasket, maybe you’d like to take a look at it and see if you can do something really cool and then put the tooth back.
We’re not going to have time today to talk about every little step. This is just a concept. Intentional replants are alive and well, and when appropriately selected, they can be viable.
All right. So you have your team and you work with microscopes, you see some failing teeth. But what I want to do is make a little quick flowchart here for you. Teeth fail, so when we’re looking at the cause, the etiology of failure, they fail because we as dentists sometimes not only don’t respect the root anatomy – notice I said the root anatomy – but we don’t sometimes even understand perfectly root canal system anatomy. So root anatomy would be like concavities, fluting, external proximations and grooves; those are the things that sometimes even though it’s on the outside it might influence what we’re doing inside. All right, so root canal systems and the anatomy of the root.
Another thing is deficiencies. Somebody might fill a canal 2mm short, somebody might miss a canal, they didn’t find it in the orifice. Sometimes we don’t see things or because of training we do things a certain way that we would consider appropriate, but it turns out that it might be the difference that made the difference. It might be why it’s failing.
So deficiencies in treatment to me are a complete difference from an iatrogenic event. Running a post out the side of the root, huge shapes that don’t respect external root anatomy – there’s that word again, root anatomy. Those are more like iatrogenics; there’s nobody teaching that anywhere in the world so dentists that are doing that aren’t following any kind of training that was introduced in their programs.
So that’s the cause of failures. I think you could take any failure in the world and put it into one of these buckets. It could even be a fractured tooth because of overzealous preparations, canals that are shaped too big for the roots that hold them, things like that.
Well what do you do? Normally what you do is you assess failure, and you might think – Ruddle almost always thinks I need to go back in the tooth non-surgically. I might see a crack through the axial wall, I might see an extra orifice that wasn’t uncovered. I could use ultrasonics, we talked about Castellucci and we talked about the SINE tips, we talked about buck tips, there’s different ways to refine the access cavity. You might be able to find something that you can address.
And then sometimes you might do the best retreatment in the world, but you inherited something that was very difficult. Your odds were not good that you could overcome the deficiencies in primary treatment or the iatrogenic event, so you’ll go right to surgery. And sometimes some clinicians find the failure and go to surgery immediately; that can be okay. I have learned over the years that it’s better for me to go back in and re-enhance the foundation. So if I am going to surgery I trust what has been done coronal to the surgical work.
But you can do these procedures and you can evaluate them, but what if a fistula persists? What if the symptoms don’t resolve? What if the lesion radiographically appears to be getting larger, not smaller, after treatment? In that case we’re going to extract and normally most dentists will say that’s enough! I’ve had it right up to here, three strikes and you’re out.
But some dentists are thinking outside the box, and based on a lot of factors – and I won’t be able to go through them all today – they might consider taking it out and putting it back in. I guess we could look at a case to get started.
Okay, so let’s look at this, it’s our first case. I’ll show three cases of replantation, intentional replantation. Sometimes things come in and you have to do a series of procedures before you even consider that. In other words, I have a big diffuse lesion in here; it’s wrapping around the apices of several roots associated with different teeth.
And so I’m looking here and I’m thinking boy, this could be a tough access because this crown is kind of sitting like this, but the roots are kind of on a bias like that. So be sure you look at your inclinations. Because if the root is going like this and the crown is like that, and I don’t even see a canal until about right in here. So this could be pretty tricky going through the posterior abutment of a bridge and then picking up the mesial systems. And then I even see something in here that might be resorption. I don’t know what that is. I have a regular canal that goes down to about here, and then I have this diffuse lesion around the distal root. So I’m thinking this root is probably more complicated than maybe its straightness – ha-ha, straightness, right? Straight roots hold hard, curved canals in the apical thirds oftentimes. So that’s kind of what I see.
When I look here I’m looking at endodontics, but it looks like maybe this tooth had surgery, maybe it’s just resorption, but that’s pretty flat. Roots are usually kind of bullet-shaped, kind of bullet-shaped. This one looks a little flat too. The patient doesn’t remember that, but they’ve had a lot of dental work and that’s what they do remember. So it’s possible with shorter roots, kind of blunted roots.
And then I look at the distance from here to here, the distance from here to here, and they’re not the same. So there could be another system in that tooth, but it could be a blocked canal apically, it could have been a transported canal, it could be the ledge that became the rip and the tear.
So I’m seeing that with that tooth, and the patient wants both teeth. This is a second molar, this is a third molar, and lots of times patients want to keep third molars, especially if they’re in occlusion with the opposing tooth.
So we go ahead and do one visit. It was a longer appointment because it’s a tough case, long, long roots. But notice the curvature, you can see it right to here, see that canal coming down quite nicely. But then you’ve got a branch here and a branch there, and you can see we got those. And then we’ve got a little furcal canal to what we looked at suspiciously on the preoperative film. As I have gotten older as a clinician, things that I see that might be anatomically related, oftentimes they are. The portals of exit, remember they form adjacent to the lesions of endodontic origin.
So that takes care of that case. But what about that molar? Again, we think it’s transported; we think it’s blunted. The crown/root ratio; if you look at the crown/root ratio, the part above the bone, the part below the bone, it’s about one-to-one. So that’s not real favorable for going back in and doing surgery because of the external oblique ridge. And that makes the shelf, the buccal, shelf, and all of a sudden you’re going to be going through a lot of bone. And don’t forget it’s a third molar and don’t forget as we go posterior, the neurovascular bundle starts to swing up and it gets pretty close to being underneath these roots. So you have those kinds of considerations.
If you’re going to extract the tooth – and when I told the patient all this and I was leading them kind of towards I could make an access and go back in and explore around – the general dentist said no, I don’t think me and the patient want that. So strike one, I can’t do that. I could, but I didn’t have permission. I then could do surgery, but I don’t like the crown/root ratio, as I just said. And finally I said okay; you give me really no more choices, so why don’t we just extract the tooth? And the patient sags in the chair. But what if we could extract the tooth and do corrective work in our hand?
So that led me to this case – it wasn’t the first case I had done, but it was one of the early ones – it led to me doing about 50 intentional replantations over about a 45-year career. So you can see if you do the math, that’s not very many per year. And I lost about 8 or 9 of them, and I had many of them – that’s over 40 left – that went for over a decade, and some of them when I retired the patient still had those teeth.
So it can be a really, really good procedure, but you have to ask yourself: who should do the work? If you’re going to go ahead and extract the tooth, who should do the work? We can talk about – it could be any of these three people on the multi-disciplinary team. I stopped doing them personally because how many extractions does Ruddle do? I work in a complex, I have an oral surgeon within 100 yards. I took him out to dinner and we had a long, pleasant visit -- Dr. Ashamalla. We call him the Egyptian Madman; he could do wonderful things with his hands. And I said look. You’re used to getting in there, boom, and rolling a tooth out fast; and if it breaks you don’t care because you’ll section it and take out the other root. I want the tooth to come out in total. So I said you are way better than I am because you extract teeth every single day, multiple times. But I need atraumatic extraction.
I’ll come back to this at another time and the producer will remind me so I better be careful what I promise. But you have atraumatic techniques, especially if an implant is considered. And you can do vertical extractions so we don’t do so much back and forth, buccal/lingual rotation with our hand and the forceps. We’re doing more of a procedure where it’s like taking a cork out of a bottle. They have different kinds of forceps that can move the tooth more vertically and pull it incrementally right out the socket.
So be aware of the atraumatic, be aware of working with other members on the surgical team. The whole extraoral time we had down to about 5-7 minutes. Most of the literature was 15 minutes; some were 10 minutes. I want to talk just another sentence on the extraoral time. You need to go through the drill with your staff and with the other office, so when the patient’s over there, they’ve been seen on a consultation, they’ve been seen with me on a consultation, all the chit-chat is done. They go over there, the phone rings in our office, and they say Dr. Ashamalla is just about to deliver the tooth. Well guess what? My assistant is standing right there with a cup filled with Hank’s Balanced Salt Solution. It could be bacteriostatic physiological saline solution. But some kind of a cup and some kind of solution or reagent that is conducive to keeping that periodontal ligament and the tissue fragments vital and alive.
So you have that down. They start walking across the complex – not the patient yet, they’re still sitting in the oral surgeon’s office – the assistant’s flying across the complex about 100 yards, and she comes into the office and she’s got the tooth. We’re already there. My other assistant’s there, I’m there, and we’re ready to go to work. And things we might consider doing is having the armamentarium present. So here’s the Hank’s Balanced Salt Solution, it has some calcium, it has some magnesium chloride, it has some materials that are very, very useful to keep tissue alive.
We don’t hold the tooth in the forceps at this point. We grab with a saturated gauze with the reagent. And I want the assistant to have suction and I want this to be flooded with water. I want the tooth wet at all times, and we immediately need a diamond bur, zzzzp, you’ll do your apicoectomy and knock off roots. Sometimes you’re removing the part of the root that has the broken instrument. Sometimes you’re removing the part of the root that was transported or ripped. Sometimes you’re removing the big curve in the root that nobody could get around clinically endodontically. So the roots need to be resected quicky with a tapered diamond, and the debris will be flying around but it’s being flushed off, we have a tray down here to catch it all and we do it right over a bathtub. (If you believe that you’ll believe anything.)
Now you’ve got the roots resected and you’re looking right at them. You can stain them with Methylene Blue, Chinese Red, to just see if any dye is absorbed in other portals of exit. You might even choose to resect a little bit more. Be aware of the crown/root ratio I talked about previously.
This is the Munce Bur. Okay, I better change colors so he doesn’t panic. This is the Munce Bur – Munce, John Munce. I think it’s C. John Munce. So he’s up there in Idaho, he’s up on the mountain, he’s living the good life. This is the Munce Bur half round bur, and I like it because most teeth that have been endodontically treated, the foramens are bigger than a quarter round bur – that would be his next size smaller this way. And so I can do that, but a lot of times if you’re coming around at an angle you can just grab your ultrasonic instrument too. So these two instruments, one’s in a latch-type, slow speed handpiece. One is in a contra-angle generator, an ultrasonic generator behind it to drive it. And you could do these preps laterally, vertically, however you want to do it, but they’re done very effectively and very quickly. Remember -- extra-oral time, the clock is ticking.
So you can place your retro material. It could have been in the old days amalgam, it could have been Super EBA, it could have been bio dentine, it could have been probably not MTA because of all the flushing. I’ll probably flush the MTA right out of it because it has a set consideration at this moment; although I’ve talked to you on this very show that they have MTA coming that can set in 5 minutes, 10 minutes, 15 minutes. You choose the set time you want and then it’s pretty stable and inert; it’s not going to get flushed away rapidly like the current MTA most of us know about.
So you can put your favorite material in there, and then I want you to reach over buccal and lingual with your gloved fingers and squeeze the cortical plate because it’ll flex a little bit from the extraction that was done by the oral surgeon in my case, and that will collapse the plates a little bit. So when you put the tooth in and you push down, oftentimes in molar teeth – I didn’t say single rooted teeth – in molar teeth, they snap back into place. There’s still a lot of mobility, but the tooth won’t just fall out of their mouth. They won’t swallow it, they will not aspirate it, they can go home with it like that. You just have to give them the proper oral instructions about eating and chewing like you would any post-extraction site.
You can splint, and we’ve talked about that on other shows so I won’t really go into that. If you think the tooth is going to fall out, then you’ve got to splint it. But the splints, the bottom line is the splints must be very soft, they should allow for some mobility. We don’t want to lock that tooth down or we’re certainly going to inspire external root resorption. Either replacement resorption, or worse, inflammatory resorption. Even some of those 6, 8, 7 teeth I lost; even when I lost them, I only lost one within 30 days, inflammatory resorption. That’s because I had it bolted down, splinted, immobile. Wrong, go read Andreasen. We’ve talked about Andreasen before in traumatology; he talks a lot about this stuff, the intentional replant. So those are some of the considerations. Splint if you have to, but it’s a softer splint. You can snap them in and most times that’ll hold it.
So if we just fire out and go forward, this is at about 10 years; this is at about a 10-year recall. We’ll get back to something a little better maybe -- 10-year. And you can see the bone is quite nice, the furcation and all this thickened, it’s gone on, the massive lesion, it’s off the film, comes up over here. You can see it’s all grey in here, healing is ideal.
So that’s an example where we kept the tooth and did a 10-minute, a less than 10-minute procedure, and I had the right team. I had the oral surgeon to come across and pick up my deficiencies and my oral surgery skills, so we had the best person to take the tooth out. If the tooth cracks or breaks they’re in the oral surgeon’s office. Who’s better to go after a root tip? You know we talked about prison dentistry earlier where we said one of the few things they refer is third molars. And when they are in the clinic in the prison, BOP, Bureau of Prisons; when they break a root tip, sometimes because of experience they have to refer that case out. So if you have anything break, they’re in the right office; they’re in the office of the oral surgeon.
All right. I’ve shown this case before, but I’m showing it just for fun again. You need to see different ideas and this is an idea where we have a big post. This is a post that’s deviated; you can see it’s deviated in the straight-on angle where we’re basically breaking the contacts perfectly right in here, but a little overlap in here, a little overlap. And you can see when we move the cone a little bit and we come more from the mesial, now we can really see that post is deviating much more than a single image would have ever disclosed.
So I have said for a long time now, take three preoperative views, moving the cone in the horizontal angle up to 30° mesial – you don’t have to go 10, up to 30 – come back to central, straight-on, and go 30° to the distal, and those three views will give you a lot more information. Of course if you have a CBCT you’re going to take that immediately; I still think there’s a benefit of more than a single preoperative digital x-ray.
So we’ve got a sinus tract, massive lesion, previous endodontics, it’s a dentist’s wife. The dentist is always there too; it made it real pleasant. He wanted me to correct the post. I was finally able to convince him this post was a little off axis. He didn’t agree here, he thought it was perfect, never saw bleeding. That doesn’t mean anything does it? Look at the result. Years later, a huge lesion on his wife.
So here a combination flap is coming up. We reflected, you can see the osseous window, we’re taking out a massive wad of granulation tissue that’s in that black lesion radiographically. You can see from kind of a lingual view, we can see the root up in here, we can see a big clump. When you see a big clump – not like tags, but a clump of tissue – remember back to the x-ray; that’s the post and that’s granulation tissue in the bone over the post. We don’t want to scrape roots, we just said that on the previous case. Do not scrape roots, just flood the roots with copious amounts of Hank’s Balanced Salt Solution, keep everything moist, the root moist, the sharpies fibers moist, the granulation tissue moist, and all the tags of tissue; keep them all alive.
So it became clear I could not approach it. I could no approach the defect. It was around the mesial, but worse, it was on the palatal side. And I’m just showing you different views; now you’re looking straight facial. You can see the leakage, you can see the staining of the gutta-percha; so not only was the post out, but that is overt, frank, visual leakage. Notice the black rim around the pink gutta-percha.
And now when I scrape off some of this, some of this, just get it out, then you can see there’s the post perf. This is directly, almost straight lingual. This is the lingual surface, the palatal surface. So there’s no way surgically you can approach this unless you cut the whole root down, and then you might be able to bevel the root a little bit further and get the post tucked back inside the confines of the radicular space. You might be able to do that, but then you don’t have any tooth to replant. So this shows the power of being able to visualize it and do something about it.
So there’s the apical repair, there’s the lateral repair, lateral repair, apical repair. This required a splint. This is a conical shaped root so I told you not splint when they snap back into place. This went back to place easily, but guess what? It started to just kind of creep and drift a little bit incisally; it wanted to come out. So we did have to do a soft splint on the facial just to kind of hold it in there.
And then here we are a little bit later in time and you can see where we had the massive, not only apical but lateral lesion. You can see how the bone’s tucked back in, it’s nice and tight, and it is a regenerative procedure if properly performed. So when we do endodontics right we can grow bone. If we need an implant, this is a better site to put an implant in, even if we lost the tooth, than over here, over her on the left.
Okay, so get the splint off in about 30 days, get it out of there. Let the tooth start to function a little bit. No biting into apples, no shearing bread like a croissant or something with hard crust. Just be careful and let everything tighten up, get the splint off and there they are. So here they are at the same day, and we see a little bit of recession. That’s going to be okay because when this lady smiles we do not have a high lip line. We’re kind of like this so we’re going to be okay. But you have to talk about that before, because what if they did have a high lip line? Then you have to tell them that sometimes when we do an intentional replant there’ll be a little bit of osseous remodeling and there’ll be a little bit of gingival recession and you might show a little bit below – or above in this case – the margin of the crown.
Okay, the last case will go fast because it’s an abortion. This is an example – so I tried to give you three examples. Deficiencies in treatment aren’t considered necessarily huge errors; that’s just probably prior training. And then we talked about the iatrogenics. Nobody teaches this in dental school. Nobody talks about making an autobahn to the freeway, straight as an arrow, go as fast as you can. We have to remember, when you see this little line in here, that little black line; you see this and then you pick it up again down here. That is in a cross-section, that’s the furcation and this shape is like this. So the shape has exceeded the confines and the boundary lines of the root itself.
So I can’t do anything here. Of course apically the root’s over here, the foramen is over here, there’s two canals so I don’t know if there’s one or two. But it’s been transported and ripped here, it’s been ripped, torn and perforated furcally – that’s a stripper if you want the terminology. And then nothing there. And then here I’m thinking well, I have an infrabony pocket, I have a little furcal thing so that’s probably how the bone comes. And I’m thinking I’d better retreat this canal, because what if there’s a branch that comes off and that would explain that. So if you’re going to extract the tooth you might be able to see it; you might not be able to see it. There might be a tissue tag over it, and again you’re not going to curette the root, because by curetting the root you’re going to increase the almost 100% likelihood that the tooth will be lost through resorption.
So I’m going to go in the distal root. I’m not trying to do a Cliff Ruddle job on this; I’m just going in there to find another canal. There’s two canals. I’m not really worried about getting down around to the end of the root because the treatment plan is to remove the tooth, apicoectomy. So I just need to shape somewhat short and get a nice, tight pack, and that’s what we did.
So outside the mouth you can make these big repairs. Now you can see perfectly the concavity. That’s the concavity on the back side of that root, the distal aspect of the mesial root. And you can see we’ve got it corked apically, two systems that merged apically apparently, but they kind of diverged to go their separate ways as I prepped up the root coronally, extra orally. And there it is.
So again, this is another 10-year result. You can see the tissue, I think, piled up here if you look really carefully. But here’s the bone level, and this bone level somehow scallops back up and gets back on up to there. So I’ve got good, tight furcal bone, good tight furcal bone. I’ve got distal healing, apical healing, and that is the power, ladies and gentlemen, girls and boys, hobos and tramps. Intentional replants can be a very, very excellent choice on a strategic tooth that has the kind of root anatomy that’s conducive to an extraction. Keep it in mind and keep it on your radar.
CLOSE: What Does Phyllis Think? – Facing Challenges
Okay, so it’s time for another episode of What Phyllis Thinks; or for me it’s what Mom thinks. Phyllis has been doing this for 12 seasons now, so we have to assume that it’s becoming a lot easier for her. But is it really? Or is she just doing hard better? And if you don’t know what I’m referring to, I’m referring to a podcast we did recently where we showed a speech by Kara Lawson who is the Duke women’s basketball coach, and she talked about how we’re waiting for things to get easier but they never do; we just learn how to do hard better. So with that in mind, we’re going to ask Phyllis some questions about how she reacts to challenges, and also some of her observations about how some of her family members are reacting to current challenges. Okay?
Yes.
All right. My first question for you is would you say you are the kind of person who procrastinates, maybe out of insecurity, and hope stuff will get easier? Or do you feel at this point in your life that you do hard pretty well and tackle projects with confidence?
It’s kind of a multiple answer. I definitely am not a procrastinator. But I notice that my energy level as I’ve gotten a little older is not quite what I expect of myself. And so I’m working on that thinking, because a lot of it I know is thinking. But physically the energy is a little bit different. And I’ve talked to a few friends who are the same age and we have the same stories. About 3:00 in the afternoon we’re going what happened? We need to keep going!
You know it’s actually funny you say that, because I sometimes feel tired in the afternoon and I think of you. I think of all the stuff you do and I think to myself, why does Mom never get tired? I actually think this sometimes at home when I’m tired.
Yeah, well one time when she left the office we replaced her with three women.
That is what I expect.
That is your expectation.
So maybe rather than hard better, she needs to do energy better.
I need to delegate.
Well I like that you’re training your thinking to actually trick yourself into thinking you have tons of energy.
Exactly.
That’s right.
All right. Well currently your granddaughter Sophia is hiking the Pacific Crest Trail -- starting at the US/Canadian border in Washington State and finishing at the California/Mexico border. And it’s going to take her four months; she’s already been gone I think like two months now.
A good month and a half, yeah -- approaching two months.
All right, so what do you think about this endeavor she’s on?
Well going into it we kept thinking she wasn’t going to do it. The more we heard about it it was like no way. I mean can you imagine being out there four months, roughing it in a tent every night? I mean it’s just crazy. I can’t imagine doing it myself. I like camping, but I don’t like the hiking. I don’t like the surviving thing.
So it’s been an interesting journey the last month and a half for our whole family, hearing her tales of the trail.
How do we hear about it?
From Lori.
Well tell the audience.
Over satellite. She has a satellite phone and she has her cell phone. So when she’s within cell distance of a tower she can use her regular phone. But the satellite, I text her everyday on her satellite phone and sometimes I don’t hear back. And I’m the grandma so I’m a little bit removed, but poor Lori and Monty.
Do you ever feel worried personally?
Every night. Every night I think about her sometime in the night. So it’s been quite a journey for all of us.
Okay, so why do you think Sophia might want to do something like this?
Well first I thought she was just crazy. But then I thought okay, probably not that. But she is so competitive.
She’s a warrior.
She loves running and trail running, and somebody probably suggested and started talking about it. She had read the book, Wild. I don’t think she had seen the movie, but it was something that she was interested in doing and she loved the challenge and here we are.
I have to say that when I first heard about it I thought also this is crazy. But then when I’ve now seen some updates, it actually sounds like I’m thinking now, God, maybe I’ll do this myself. It sounds pretty exciting.
You could.
Okay, next question. Sophia started off with someone else. That person is no longer – she’s alive, she’s no longer hiking with her. So Sophia is doing it alone. So what do you think about doing all of this alone?
It’s worrisome. But I understand her personality and her competitiveness. She competes against herself more than anybody else.
And it doesn’t hurt that she carries a Smith & Wesson.
That helps too, and a big knife. (We’re kidding.) That would be nice if she did.
Yeah, she doesn’t seem that worried to do it by herself.
No, I think she probably has moments where she feels alone and worried about stuff. But in general she likes the challenge against her own perceptions.
And I guess I’ve also heard there’s other people she runs into.
Every day.
And she’s met some people, so it’s not like she’s completely isolated.
She’s hiking alone because she’s going from north to south. Most of the hikers are going from south to north. But she interfaces with people every day to some extent. I think it would be a rare day that she doesn’t see anybody. So we’ve kind of adjusted to that’s how it’s going to be.
Okay, well let’s go on now to something that recently involved you and Dad. You recently had a German group come for dad to teach and interact with, and it required a lot of planning and organization. You used to do this kind of thing regularly in the past when you gave the seminars, but in recent years not so much. Did you feel overwhelmed or stressed out when you were faced with this challenge?
Yes. We were so rusty. Lori and I put everything in storage when we moved the office home, and we haven’t done a course for five years. So in theory when we agreed to do it, it all sounded very doable because we had done it so much. But when it came down to the details of finding everything it was like where is that?
So I went out to storage one day looking for stuff, had a whole story about that, and just finding a way to pull it all together was a little overwhelming after not doing it for so long.
But did you – you knew you had to do it so you just kind of toughened up and did it?
Just did it, yes.
And then as you were doing it did you find it seeming more doable?
Yes, and thought of ideas for the next time. So I would say it could happen again and we would be definitely ready.
Was it okay to have Lori help you with the hotel, the food, the setup?
Thank God for Lori! She loves the detail part of it.
They’re a pretty good team, huh?
Yeah, yeah.
Okay, well the meeting turned out very successful. Do you think that when you succeed at something that seems overwhelming or scary or challenging that success maybe feels extra inspiring?
The satisfaction, and just making people happy. That makes it all worth it. So the hardest part for me was the long days. We would get up about 4:30, get down to the hotel, and then we had clear through the evening to about 10:00 p.m. for dinner. So it was a long two days, and I’m thinking about how to tweak that another time. But long, long days.
So no risk it, no biscuit? I think it’s Don Arian’s, or Bruce Arian’s expression that I say a lot at home and I get told to stop.
Okay, next question. One of your grandsons, Luca, recently traveled across the country to Florida to play a tennis tournament, and then also recently to Michigan for another tennis tournament. So Lori, who is terrified of flying took him. Do you have any opinions about this, and maybe what kind of pressure Luca might have been feeling as well?
My journey of traveling days, and the whole flying thing; I had to go through the same thing myself. And it takes a long time to be comfortable with that lifestyle. So I think it’s great he wants to be a tennis player, he wants to be out there and go everywhere in the world and play. And this is part of the journey is learning how to do that -- the stuff behind playing tennis. He loves the courts and all that, but the whole rest of the time zones and all that stuff.
It sounds a little bit like the German course. There’s the course and then there’s the peripheral stuff. For me there was the travel, and that’s a whole story, and then you just get up there and give your lecture. So Luca’s learning a lot.
Yes. You had to do it, I had to do it. I mean there’s all this other stuff that goes into what you want to be in life, and you just have to do it.
Just so the audience gets a small glimpse. California, Santa Barbara, about 75° would be a high. Florida would be like 90-95 with about the same humidity, so there’s a whole different demand. Michigan you’re thinking is north, way better. It is blistering hot in Michigan and they have a lot of humidity because of the lakes. So he’s learning about time changes.
Yeah, and then I don’t know if he might feel a little bit like I’m making mom take me here, we’re flying all these miles and we’re staying in a hotel, I’d better do well. I mean does he have that kind of pressure?
I’m sure he does. Plus like Sophia, he drives himself. So he has to learn how to handle that too. That’s all part of it.
Phyllis generally tells him if you don’t win, forget the return ticket home.
Exactly.
Yeah, maybe you just don’t have one outcome that you need. You kind of look at different possibilities and what you can learn from those, so it’s not just about getting a certain outcome.
He’s really good at putting things into balance.
Okay, I think we have time for one more question. So Eva, your other granddaughter, works in a hair salon and often has to do hair retreatment. Meaning another stylist messed up someone’s hair and she has to fix it. And Eva is actually very good at this. She will tell me she was insecure or worried during the procedure, but she also was trying to project confidence because she doesn’t want her client to be worried and see that she’s a little nervous herself. So do you ever feel like this?
I remember in the office we had to deal with that a lot with endo retreatment stuff. You would see some of the things that would come in and I’d be going I don’t think it’s possible. And he would just take it down piece by piece by piece, and it was possible. And so I’m very familiar with that aspect. Then when you’re working with the public like she does with the hair thing, it can be very intimidating. But it’s just one step at a time. You break it down, you know you can do it. And if you can’t, you tell them; I’m sorry, I can’t do this. And then you’re fine.
You know, what you’re saying is I’m so proud of her. Everybody thinks oh, cosmetology; chemicals and all that stuff. But she’s learning communication. And she’s learning to clarify her communication, because there’s what people hear and what you said and they’re not always the same. So she’s learning to repeat back and really understand what their biggest chief complaint is, and I think that’s going to help her all through life.
And she has a real good feel about her when she’s talking to people. And she sees things, and that’s good. She has good antenna.
Yeah, being realistic so that they know what to expect. Not promising success and then –
Don’t over promise.
Right. And I also like what you said about the situation as a whole might seem really challenging and scary. But when you just start breaking it down -
One hair at a time.
Yeah, one thing at a time. Then maybe it starts to seem more manageable.
Yes. And keep the fee up. That’s one thing I learned about in the dental office; keep the fee up.
Okay. We can just leave that as your final advice if you’d like.
It works in all aspects of life.
It is retreatment.
Yes, it works in all aspects of life. Think about the fee.
Okay, well thank you for joining us for What Phyllis Thinks again.
You’re welcome!
Good job.
We love having you on. Do you feel nervous when we tell you it’s time for What Phyllis Thinks?
Not too--I did at first, but not too much. I’m pretty good at coming up with things to say.
So she’s doing hard better.
Yes.
All right. Well thank you and that’s our show for today. See you next time on The Ruddle Show.